At 2016 Summit, Field Tackles AD-Related Dementias One By One
Quick Links
While it’s not the $2 billion researchers are asking for, at $991 million, this year’s National Institutes of Health budget for studies on Alzheimer’s disease and related dementias has never been higher. How to get the biggest bang for the newfound buck? On March 29 and 30, the National Institute of Neurological Disorders and Stroke (NINDS) gathered experts at NIH in Bethesda, Maryland, to put their heads together and update the field’s overall strategy. This Alzheimer’s Disease-Related Dementias 2016 Summit gave the public a chance see where the field stands and to weigh in on expert recommendations, which will help revise the National Plan to Address Alzheimer’s Disease.
At the summit, researchers addressed challenges that span all dementias (see Part 1 of this series). They then surveyed the status of three separate groups of diseases: Lewy body dementias, frontotemporal lobar degeneration (FTLD), and what is now termed vascular contributions to cognitive impairment and dementia (VCID). Next steps differ for each one, but some broader themes emerged, especially defining the stages of early disease and coordinating research efforts. Representatives of individual working groups summarized progress made since the 2013 ADRD summit and outlined future research priorities (the full list is available here).
Lewy Body Dementias
As a group, Lewy body dementias (LBD) have in common the accumulation of aggregates made up principally of α-synuclein. This group of diseases includes Parkinson’s disease dementia (PDD), which starts with movement problems and gradually adds cognitive impairment, and dementia with Lewy bodies (DLB), in which dementia accompanies movement problems from the beginning.
Topping the priority list at the 2013 summit, and again this year, were clinical trials of repurposed drugs, investigational compounds, or non-pharmacological methods to treat the symptoms of LBD, said Jennifer Goldman, Rush University Medical Center, Chicago. Few advances have been made on that front. In the past three years, a handful of clinical trials has been completed for DLB, mostly for drugs used in Alzheimer’s (Ikeda et al., 2013; Ikeda et al., 2015). Donepezil has since been approved for DLB in Japan, making it the first drug licensed for the disorder worldwide. Smaller trials examined have compounds such as armodafinil for daytime sleepiness and nilotinib to break up α-synuclein deposits (Dec 2015 conference news; Nov 2015 news). A pilot trial is exploring whether deep-brain stimulation of the bilateral nucleus basalis of Meynert improves memory and thinking. The upcoming HEADWAY trial will examine whether RVT-101 improves cognition in DLB. Two other trials will test whether nelotanserin reduces visual hallucinations and REM sleep behavior disorder in people with DLB.
Three clinical trials have targeted PDD, Goldman said, one finding that rivastigmine is safe for this disorder, another that memantine lessens caregiver burden, and another that pimavanserin may relieve psychosis (Emre et al., 2014; Leroi et al., 2014; Cummings et al., 2013). Pimavanserin is now widely expected to become the first antipsychotic approved in a neurologic disease (Apr 2016 news). Ongoing studies are examining SYN-120 and an increased dose of donepezil for cognition. Goldman said that the committee recommends keeping therapy trials as the main priority.
Her working group also agreed that researchers need a better handle on early disease and diagnoses. Longitudinal DLB cohorts that collect clinical, biological, and imaging data on patients from early disease to autopsy will help, Goldman said. One way to get that data is by expanding the Parkinson’s Disease Biomarkers Program at NINDS to include clinical data and biological specimens from patients with PDD and DLB. NIH recently issued a request for applications for that purpose. Applications are due May 10.
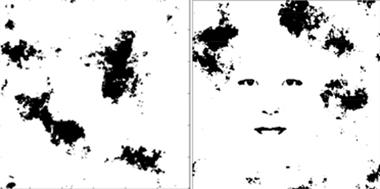
Man in the Moon?
In the pareidolia test, people with DLB tend to misinterprete random stimuli. They see faces where there are none (left), or miss faces that are there (right). [Courtesy of Yoshiyuki Nishio, Tohoku University.]
Another new resource is the DLB module for the National Alzheimer’s Coordinating Center (NACC). Led by James Galvin, Florida Atlantic University, Boca Raton, scientists are working on this already. This standardized test battery will allow all Alzheimer’s Disease Centers across the United States to include DLB and PDD patients in their longitudinal studies and pool their results in a large, widely available database. The current draft module compiles neuropsychological tests, measures of behavior and mood, and other clinical tools that capture the motor and non-motor symptoms of PDD and DLB. For instance, the noise pareidolia test assesses a person’s tendency to hallucinate by whether or not they see faces among random visual information (noise). The draft module will soon be ready to distribute to ADCs for their review, Galvin said.
The committee further recommended compiling an inventory of available autopsied LBD brains to prepare for large, coordinated studies. It also urged researchers to find new genetic variants for LBD, come up with biomarkers and research models, and discover disease-modifying therapies. (For recent research updates on DLB, see Dec 2015 conference series).
Frontotemporal Lobar Degeneration
FTLD are a heterogeneous group of diseases unified by a common finding of atrophy in the frontal and temporal lobes of the brain. They can have a variety of underlying protein pathologies, including tau, TDP-43, or FUS. Following a string of genetic discoveries, scientists are now in the midst of an explosion of work to discover the mechanisms of disease in this especially diverse group of disorders. “We are understanding the pathways involved in more detail than ever before,” said David Holtzman, Washington University in St. Louis. Many researchers agreed broadly that progress in the molecular biology of FTD is so rapid they are having trouble keeping up.
One pressing priority is working out the mechanism for tau toxicity and spread, said Virginia Lee, University of Pennsylvania, Philadelphia. In the past three years, researchers have made headway in cellular and rodent models. Previous work from the lab of Marc Diamond, who is now at the University of Texas Southwestern Medical Center in Dallas, demonstrated that different strains of misfolded tau give rise to different tauopathies (May 2014 news). At the same time, Brad Hyman’s group at Massachusetts General Hospital, Boston, implicated a rare high molecular weight isoform of tau in propagation, and cortical Aβ was found to accelerate spread of tau beyond the entorhinal cortex (Takeda et al., 2015; Pooler et al., 2015). Karen Duff, Columbia University Medical Center, New York, has found that more neural activity in the hippocampus of a transgenic mouse model accelerates the spread of tau. “This is an exciting new target for therapy,” Lee told the audience. Holtzman agreed, saying “The spreading issue is very attractive. You could theoretically see how that is targetable in the near term.” Several companies have therapeutic antibodies in Phase 1 trials, with the idea that snagging tau outside the cell, before it can be passed along, could stall a toxic spread.
Another major goal of the field is to figure out why C9ORF72 hexanucleotide repeat expansions and mutations in the progranulin gene are toxic. Leonard Petrucelli, Mayo Clinic, Jacksonville, Florida, summarized recent developments in C9ORF72. Do the expansions disrupt the normal function of C9OFR72, are the tangles of RNA and RNA-binding proteins (RNA foci) that result from their transcription toxic, or is it the unusual translated repeat dipeptides? This is very much ongoing research, Petrucelli said. The past three years of work have shown that C9ORF72, along with progranulin and TREM2, a gene associated with Alzheimer’s disease, are all heavily expressed in microglia. “Clearly our emphasis over the next few years will be the role these genes have in microglial involvement, and whether they sensitize cells to the aberrant accumulation of proteins.” Transgenic mice that have been developed to model the expansion will be key, he told the audience. In one overexpression model, Petrucelli’s group linked the C9ORF72 repeat expansion with TDP-43 inclusions, an underlying pathology in people with the expansion (Chew et al., 2015). “It gives a lot of hope that if you can target the C9ORF repeat expansion, hopefully the underlying pathology will be ameliorated as well,” Petrucelli said.
Researchers are likewise working to figure out what is so toxic about the principally nuclear TDP-43 relocating to the cytoplasm and aggregating there, said Manuela Neumann, German Center for Neurodegenerative Diseases, Tübingen. Animal models point to loss of normal TDP-43 function but cannot rule out a toxic role for its cytoplasmic inclusions. The field needs to learn more about what TDP-43 does normally, about how the gene mutations interfere, and about why the protein moves out to the cytoplasm. Another key question is what makes TDP-43 aggregate once there. Current in vitro studies suggest that when the protein concentration rises, a “second hit” causes stress granules to form, which recruit TDP-43 and lead to its aggregation. In vivo evidence of this multiple-hit hypothesis is needed, as well as determining whether misfolded TDP-43 templates further misfolding and if guiding TDP-43 back into the nucleus could be therapeutic.
Other scientists are plugging away at the genetics of FTDs, searching for more causative and risk genes. Some new ones have come from genome-wide association studies, said Rosa Rademakers at the Mayo Clinic in Jacksonville. The first GWAS on corticobasal degeneration, a type of FTD, was completed last year (Kouri et al., 2015). It returned a hit in MOBP, short for myelin-associated oligodendrocyte basic protein, which was recently implicated in progressive supranuclear palsy. This suggests the two disorders share some genetic factors. An exome sequencing study of FTD found a novel gene already associated with amyotrophic lateral sclerosis, TANK-Binding Kinase 1 (TBK1), important for autophagy and inflammation (Cirulli et al., 2015; Pottier et al., 2015). As the field moves toward whole-exome and whole-genome sequencing, new genes will point to molecular pathways, Rademakers said. The committee recommended genotyping more FTD patients to try to identify more variants.
Researchers at the summit said they urgently need biomarkers that differentiate between FTLD-tau, -TDP, and –FUS. FTLD is the pathological term that corresponds to the clinical term FTD. Being able to distinguishing these pathological subtypes will refine recruitment into clinical trials and identify which patients will benefit from which future therapies. One way to tell pathologies apart may come from positron emission tomography (PET) imaging with tau ligands. This area is evolving rapidly as researchers are realizing that the best-studied tracer thus far, AV1451, may work less well in FTD than AD, and a handful of new tau tracers are entering clinical study. Brad Dickerson, Massachusetts General Hospital, Boston, highlighted recent research with AV1451 in FTLD. AV1451 binds in patients with the MAPT mutation MAPT301L, who likely have tau pathology, in areas where there is atrophy. The signal also appeared in a patient 10 years before their predicted age of onset, suggesting this could work as a preclinical biomarker. However, the AV1451 signal also shows up in people with GRN and C9ORF72 mutations, who are not expected to have tauopathy. What is AV1451 sticking to in those patients? Only brain autopsies can answer that. “We need to increase resources to validate these tracers in vivo and postmortem to understand what the ligands are binding to,” Dickerson said.
International FTD clinical trial networks that collect clinical, genetic, and biomarker data also top the list of research priorities in FTD. Ideally, these could grow out of natural history networks that track FTD by following familial FTD patients from health to disease, and sporadic patients from the earliest symptoms to advanced disease. The Genetic Frontotemporal Dementia Initiative (GENFI), the Longitudinal Evaluation of Familial Frontotemporal Dementia Subjects (LEFFTDS), and the Advancing Research and Treatment for Frontotemporal Lobar Degeneration Consortium (ARTFL) are working to accomplish these goals, said Adam Boxer, University of California, San Francisco (Nov 2014 conference news; Nov 2014 conference news).
Vascular Contributions to Cognitive Impairment and Dementia
Lastly, researchers reviewed progress and goals for VCID, which is the new term encompassing the role of vascular disease in neurodegeneration and dementia. The working group first focused on biomarkers of small vessel diseases, that is, arteriolosclerosis caused by chronic hypertension, diabetes, or hypercholesterolemia; as well as cerebral amyloid angiopathy from amyloid buildup around arterioles. Researchers need more non-invasive markers of the subclinical vascular processes that slowly erode the brain’s vascular integrity and lead to dementia. One recent success came with development of 7T magnetic resonance imaging (MRI), said Jin-Moo Lee at Washington University. Its high resolution allows researchers to see microinfarcts in living people. Such tiny strokes occur with alarming frequency in small-vessel diseases, he said. Other techniques in development aim to measure the enlarging space around cerebral blood vessels that occurs in aging and hypertension, as well as functional connectivity in mice.
Researchers need to develop animal models to mimic destructive vascular processes, said Lee. For instance, Andrew Shih at the Medical University of South Carolina, Charleston, has found that he can use lasers to create artificial microinfarcts in small blood vessels of mice, and track with serial MRI as discrete lesions run together. This may provide a construct to understand how microinfarcts become large-scale regions of damage that lead to dementia, said Lee.
Once again at this summit, a theme was collaboration, as challenges such as biomarker development, or big-data analysis, appear to be too complex for individual groups to solve. One such project that grew out of the 2013 summit and is now coming to fruition is the Molecular Mechanisms of the Vascular Etiology of Alzheimer’s Disease (M²OVE-AD) Consortium, led by NIA and NINDS, is inspired by the Accelerating Medicines Project (AMP) for AD (Feb 2014 news). The five-year, $30-million M²OVE-AD comprises five projects involving more than a dozen research teams. It will collect multiple layers of molecular data—genomics, proteomics, and metabolomics—from autopsied brains of AD patients, as well as blood and plasma of people in vascular studies, to find out how vascular risk factors influence Alzheimer’s. This data will be shared with scientists in real time, hopefully resulting in reproducible, transparent, and translatable research, said Suzanne Craft, Wake Forest School of Medicine, Winston Salem, North Carolina.
Another underlying theme in VCID research involves the neurovascular unit—the finely structured interface between neurons and blood vessels in the brain. Researchers have been surprised to find that a vessel’s cellular arrangement changes depending on where it is in the brain, said Costantino Iadecola, Weill Cornell Medical College, New York. After the blood vessels enter the brain and extend over the pia, they penetrate into the parenchyma and eventually arborize into capillaries. Along the way, the cellular anatomy of the neurovascular unit changes. For instance, near the top of the brain, extra parenchymal arterioles are somewhat elastic, get nerve input from outside the brain, and have a defined perivascular space around vessels. By contrast, intraparenchymal arterioles lose the input from perivascular nerves and have no perivascular space. Thus, different sections of the same vessel are vulnerable to different pathogenic processes, Iadecola said. The turbulent blood flow in the main vessels entering the brain makes them prone to atherosclerosis, while smaller vessels are susceptible to microinfarcts and microbleeds. These processes lead to different kinds of dementia. New approaches to studying the neurovascular unit, such as by modeling it on a chip (see image below) will allow researchers to understand the interplay of the different NVU components and how they cause dementia, said Iadecola.

Chip Off the Old Brain. This chip models the neurovascular microenvironment, with various cell types and barriers, as well as the flow of blood and cerebrospinal fluid. [Alcendor et al., 2013. Stem Cell Research & Therapy.]
Does this research translate into concrete actions people can take now to reduce their dementia risk? Perhaps, said Steven Greenberg, Massachusetts General Hospital. Both Greenberg and NINDS director Walter Koroshetz called the widely reported recent decline in age-adjusted incidence of dementia an “unclaimed victory” of vascular research (Feb 2016 news). “It’s maybe the most exciting public health finding to emerge,” Greenberg told the audience. This reduction could “mitigate the tsunami” of dementia cases projected for the near future, he said.
The reason for this decline in dementia incidence remains unclear, Sudha Seshadri of Boston University told the audience, but it occurred during the time period when smoking, cholesterol levels, and stroke all decreased. The summit committee’s guidelines urge longitudinal trials on lifestyle change with years of follow-up, similar to the multi-domain intervention trials ongoing in Europe to further explore this relationship (Nov 2015 conference news). More synergies could be found in feeding vascular and AD mouse models different diets and aging them. “If vascular risk and a diagnosis of Alzheimer’s are linked, and it looks like they are, then by getting risk factors under control we could reduce risk of AD and related dementias,” Koroshetz told Alzforum.
In terms of research funding, this means that studies on pathogenic mechanisms and preclinical biomarkers of VCID remain important priorities, scientists agreed. At the same time, the overall link between vascular risk factors and dementia has reached such broad consensus that renewed effort and creativity could be directed toward public awareness. Roderick Corriveau, NINDS, pointed to Mind Your Risks, a campaign NINDS launched this February to educate physicians and laypeople about the importance of controlling hypertension to stave off dementia. It proposes a number of heart-healthy measures, such as lowering cholesterol, kicking a smoking habit, and keeping active. “We’ve been advising our patients for 20 years to be heart-healthy to lower their dementia risk,” Holtzman said. “We now have better data that that’s the right message.”
For video recordings of day 1 and day 2 of this event, visit the NIH Center for Information Technology website.—Gwyneth Dickey Zakaib
References
News Citations
- Dementia with Lewy Bodies: Is the Research Ready For Clinical Trials
- Potential Parkinson’s Treatments Target α-Synuclein, Cell Replacement
- Pimavanserin Nears Approval to Treat Psychosis in Parkinson’s
- Like Prions, Tau Strains Are True to Form
- Meet the Artful Leftie: NIH Jump-Starts U.S.-Canadian FTLD Cohorts
- First Data from GENFI1: Brain’s Insula Region Shrinks A Decade Before FTD
- New Initiative AMPs Up Alzheimer’s Research
- Falling Dementia Rates in U.S. and Europe Sharpen Focus on Lifestyle
- Health Interventions Boost Cognition—But Do They Delay Dementia?
Therapeutics Citations
Conference Coverage Series Citations
Research Models Citations
Paper Citations
- Ikeda M, Mori E, Kosaka K, Iseki E, Hashimoto M, Matsukawa N, Matsuo K, Nakagawa M, Donepezil-DLB Study Investigators. Long-term safety and efficacy of donepezil in patients with dementia with Lewy bodies: results from a 52-week, open-label, multicenter extension study. Dement Geriatr Cogn Disord. 2013;36(3-4):229-41. Epub 2013 Aug 15 PubMed.
- Ikeda M, Mori E, Matsuo K, Nakagawa M, Kosaka K. Donepezil for dementia with Lewy bodies: a randomized, placebo-controlled, confirmatory phase III trial. Alzheimers Res Ther. 2015;7(1):4. Epub 2015 Feb 3 PubMed.
- Emre M, Poewe W, De Deyn PP, Barone P, Kulisevsky J, Pourcher E, van Laar T, Storch A, Micheli F, Burn D, Durif F, Pahwa R, Callegari F, Tenenbaum N, Strohmaier C. Long-term safety of rivastigmine in parkinson disease dementia: an open-label, randomized study. Clin Neuropharmacol. 2014 Jan-Feb;37(1):9-16. PubMed.
- Leroi I, Atkinson R, Overshott R. Memantine improves goal attainment and reduces caregiver burden in Parkinson's disease with dementia. Int J Geriatr Psychiatry. 2014 Feb 7; PubMed.
- Cummings J, Isaacson S, Mills R, Williams H, Chi-Burris K, Corbett A, Dhall R, Ballard C. Pimavanserin for patients with Parkinson's disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet. 2013 Oct 31; PubMed.
- Takeda S, Wegmann S, Cho H, DeVos SL, Commins C, Roe AD, Nicholls SB, Carlson GA, Pitstick R, Nobuhara CK, Costantino I, Frosch MP, Müller DJ, Irimia D, Hyman BT. Neuronal uptake and propagation of a rare phosphorylated high-molecular-weight tau derived from Alzheimer's disease brain. Nat Commun. 2015 Oct 13;6:8490. PubMed.
- Pooler AM, Polydoro M, Maury EA, Nicholls SB, Reddy SM, Wegmann S, William C, Saqran L, Cagsal-Getkin O, Pitstick R, Beier DR, Carlson GA, Spires-Jones TL, Hyman BT. Amyloid accelerates tau propagation and toxicity in a model of early Alzheimer's disease. Acta Neuropathol Commun. 2015 Mar 24;3:14. PubMed.
- Chew J, Gendron TF, Prudencio M, Sasaguri H, Zhang YJ, Castanedes-Casey M, Lee CW, Jansen-West K, Kurti A, Murray ME, Bieniek KF, Bauer PO, Whitelaw EC, Rousseau L, Stankowski JN, Stetler C, Daughrity LM, Perkerson EA, Desaro P, Johnston A, Overstreet K, Edbauer D, Rademakers R, Boylan KB, Dickson DW, Fryer JD, Petrucelli L. Neurodegeneration. C9ORF72 repeat expansions in mice cause TDP-43 pathology, neuronal loss, and behavioral deficits. Science. 2015 Jun 5;348(6239):1151-4. Epub 2015 May 14 PubMed.
- Kouri N, Ross OA, Dombroski B, Younkin CS, Serie DJ, Soto-Ortolaza A, Baker M, Finch NC, Yoon H, Kim J, Fujioka S, McLean CA, Ghetti B, Spina S, Cantwell LB, Farlow MR, Grafman J, Huey ED, Ryung Han M, Beecher S, Geller ET, Kretzschmar HA, Roeber S, Gearing M, Juncos JL, Vonsattel JP, Van Deerlin VM, Grossman M, Hurtig HI, Gross RG, Arnold SE, Trojanowski JQ, Lee VM, Wenning GK, White CL, Höglinger GU, Müller U, Devlin B, Golbe LI, Crook J, Parisi JE, Boeve BF, Josephs KA, Wszolek ZK, Uitti RJ, Graff-Radford NR, Litvan I, Younkin SG, Wang LS, Ertekin-Taner N, Rademakers R, Hakonarsen H, Schellenberg GD, Dickson DW. Genome-wide association study of corticobasal degeneration identifies risk variants shared with progressive supranuclear palsy. Nat Commun. 2015 Jun 16;6:7247. PubMed.
- Cirulli ET, Lasseigne BN, Petrovski S, Sapp PC, Dion PA, Leblond CS, Couthouis J, Lu YF, Wang Q, Krueger BJ, Ren Z, Keebler J, Han Y, Levy SE, Boone BE, Wimbish JR, Waite LL, Jones AL, Carulli JP, Day-Williams AG, Staropoli JF, Xin WW, Chesi A, Raphael AR, McKenna-Yasek D, Cady J, Vianney de Jong JM, Kenna KP, Smith BN, Topp S, Miller J, Gkazi A, FALS Sequencing Consortium, Al-Chalabi A, van den Berg LH, Veldink J, Silani V, Ticozzi N, Shaw CE, Baloh RH, Appel S, Simpson E, Lagier-Tourenne C, Pulst SM, Gibson S, Trojanowski JQ, Elman L, McCluskey L, Grossman M, Shneider NA, Chung WK, Ravits JM, Glass JD, Sims KB, Van Deerlin VM, Maniatis T, Hayes SD, Ordureau A, Swarup S, Landers J, Baas F, Allen AS, Bedlack RS, Harper JW, Gitler AD, Rouleau GA, Brown R, Harms MB, Cooper GM, Harris T, Myers RM, Goldstein DB. Exome sequencing in amyotrophic lateral sclerosis identifies risk genes and pathways. Science. 2015 Mar 27;347(6229):1436-41. Epub 2015 Feb 19 PubMed.
- Pottier C, Bieniek KF, Finch N, van de Vorst M, Baker M, Perkersen R, Brown P, Ravenscroft T, van Blitterswijk M, Nicholson AM, DeTure M, Knopman DS, Josephs KA, Parisi JE, Petersen RC, Boylan KB, Boeve BF, Graff-Radford NR, Veltman JA, Gilissen C, Murray ME, Dickson DW, Rademakers R. Whole-genome sequencing reveals important role for TBK1 and OPTN mutations in frontotemporal lobar degeneration without motor neuron disease. Acta Neuropathol. 2015 Jul;130(1):77-92. Epub 2015 May 6 PubMed.
Other Citations
External Citations
Further Reading
News
- At HAI, Researchers Explore Diagnostic Potential of a Tau Tracer
- Dementia with Lewy Bodies: Sharper Image for a Formerly Blurry Disease
- Coming in March: First MOOC on Lesser-Known Dementia Variants
- Genetics of DLB: Setting Up to Fill a Mostly Empty Canvas
- Health Interventions Boost Cognition—But Do They Delay Dementia?
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.