For α-Synuclein Immunotherapy, Is Going Later the Key?
Quick Links
α-Synuclein immunotherapy is in its infancy, with few trials posting results yet. The first two completed Phase 2s, of Biogen’s cinpanemab and Prothena and Roche’s prasinezumab, were both negative. However, while the cinpanemab study was fully negative, prasinezumab posted positive results on some secondary motor measures. At the 15th International Conference on Alzheimer’s and Parkinson’s Diseases, held virtually March 9–14, Gennaro Pagano of Roche gave researchers a first look at prespecified subgroup analyses from this study, called PASADENA. It turned out that subgroups of participants whose disease progressed fastest benefited more from prasinezumab, with more slowing of motor decline. Pagano believes this is because the signal-to-noise ratio in these subgroups was greater, allowing the small effect of prasinezumab to be discerned more readily in this slow disease.
- Prasinezumab slowed decline on those measures that changed most over one year.
- Populations with rapidly progressing disease benefited the most.
- New trial will enroll people with more advanced symptomatic disease.
“A key takeaway from PASADENA is that, in order to demonstrate the beneficial effect of an intervention designed to slow the course of a disease, there must be adequate disease progression to measure,” Pagano told Alzforum. Based on these data, Roche has started a new Phase 2b study in a more advanced, symptomatic population.
Werner Poewe of Innsbruck Medical University, Austria, agreed that patient selection is important. “Almost all trials to date, with the exception of those that target genetic forms of Parkinson’s, treat the disease as a single entity. It certainly is not,” he said in an AD/PD talk. He urged the field to develop biomarkers to distinguish different forms.
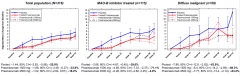
Signal-to-Noise. The slight slowing of motor decline by prasinezumab (left) was more evident in subgroups of patients whose disease progressed faster, such as those on MAO-B inhibitors (middle) and those with a more aggressive form of PD (right). [Courtesy of Roche.]
Prasinezumab recognizes the C-terminus of α-synuclein, and binds preferentially to aggregated forms. In Phase 1, the antibody entered the central nervous system but did not affect monomeric, physiological α-synuclein there (Jun 2018 news). The Phase 2 trial enrolled 316 people who were newly diagnosed with PD, with mild symptoms of slowness, rigidity, or tremor. None of them were on dopamine replacement therapy, and about one-third took monoamine oxidase-B inhibitors such as rasagiline or selegiline. For the first year, one-third of the participants received 1,500 mg of prasinezumab as a monthly infusion, one-third received 4,500 mg, and the rest placebo. Roche previously reported no effect of this yearlong intervention on the primary outcome measure, the MDS-UPDRS, but positive signals on secondaries (Apr 2020 conference news).
At AD/PD, Pagano elaborated on these findings. On the MDS-UPDRS as a whole, prasinezumab slowed decline by 14 percent. This fell short of statistical significance. However, in a planned secondary analysis, the researchers also examined each of the three parts of the MDS-UPDRS separately. Part I measures non-motor symptoms, part II activities of daily living, and part III motor symptoms. Pagano said that in early symptomatic PD, most of the decline occurs in motor symptoms; non-motor symptoms are already advanced, and ADLs are still strong. In the PASADENA cohort, participants on placebo worsened by only one point on part I over one year, compared with about 2.5 points on part II and five points on part III.
Prasinezumab had its greatest effect on part III, slowing decline by 25 percent and reaching statistical significance. Because motor abilities were scored by clinicians at each site, potentially introducing site-to-site variability, the videotaped motor assessments were also sent to a central group of raters. This prespecified central analysis returned a larger drug effect, saying prasinezumab slowed motor symptom decline by a third. This finding again implied that a higher signal-to-noise ratio rendered a treatment effect more detectable.
For all these analyses, both prasinezumab dose groups were pooled. Pagano noted that the two dosages had similar effects, and even the low dose was expected to achieve a high enough concentration in the CNS to saturate its target, based on Phase 1 data.

Digital More Sensitive? Motor decline tracked by smartphone revealed a slowing of the slope of decline on prasinezumab. [Courtesy of Roche.]
Parkinson’s is a notoriously variable disease, with patients doing better on some days than others. This means that MDS-UPDRS assessments done infrequently at a clinic are inherently noisy. For this reason, the PASADENA trial added digital motor assessments taken continuously at home using a smartwatch and smartphone. These measures were expected to be more sensitive and less variable (May 2017 conference news). Smartphone use produced a wealth of information, since there were 17 separate measures tracked either daily or every other day. With participants completing 93 percent of the requested tests, this resulted in 966,000 bits of data. For simplicity, the researchers combined several of the digital measures that assessed slowness of movement and resting tremor into a single motor score. They chose the measures expected to change the most in early PD, based on data from the Parkinson’s Progression Markers Initiative.
Prasinezumab performed similarly on this combined digital motor score as on the MDS-UPDRS part III, slowing decline by 25 percent in the pooled treatment group (see image above). In a separate talk, Kirsten Taylor of Roche broke down the details of this digital measure, noting that measures of arm and hand dexterity showed the greatest difference after treatment. For example, people taking prasinezumab were able to flip their hands from side to side more quickly and tap on their smartphone screens more accurately than people on placebo. Their smartphones also scored their hand movements throughout the day as being stronger than those of the control group.
If the effects of prasinezumab require a high signal-to-noise ratio to be visible, then subgroups of patients who decline faster should reap more easily apparent benefits. Prespecified subgroup analyses supported this, Pagano said. In one such analysis, researchers divided the cohort into people who are on concomitant MAO-B therapy and those who aren’t. Because MAO-B inhibitors are prescribed to Parkinson’s patients with more symptoms, this group is likely to have more advanced or faster-progressing disease. Indeed, the subgroup of 115 participants taking these medicines worsened by 7 points per year on the MDS-UPDRS part III, rather than 5. Prasinezumab slowed their decline by 40 percent.
Parkinson’s disease can also be classified by its severity. People whose decline is in the lower 75th percentile on all measures are considered to have “mild motor-predominant” disease, while those with several motor and non-motor scores in the top 25th percentile are labeled as having “diffuse malignant disease.” Everyone else falls into the intermediate category. In the PASADENA cohort, the 15 participants with diffuse malignant disease who were on placebo declined by 12 points on the MDS-UPDRS part III. For the 44 with diffuse malignant disease who received prasinezumab, this decline slowed by 64 percent.
“Based on these findings, we decided to invest further in this compound,” Pagano said. Roche has started the Phase 2b PADOVA study, which will enroll 575 people who are on levodopa therapy, indicative of more advanced PD. In the PASADENA trial, if a participant worsened enough to start dopamine therapy, their subsequent data was not included. The PADOVA trial will run for 18 months, with the primary outcome measure being how long it takes each participant to worsen by 5 points on the MDS-UPDRS part III. A change of 5 points is considered clinically meaningful, Pagano noted.
There is more data to come from the PASADENA trial, as well. In its second year, all participants went on prasinezumab, including those who were formerly on placebo. Data collection from that portion of the trial recently wrapped up, and the findings are being analyzed now, Pagano said. These data will help answer the question of whether prasinezumab slowed underlying disease progression, or merely reduced symptoms. If the former, people who were on drug in the first part of the study would be expected to maintain an advantage over those who were on placebo.
Other researchers welcomed the data from PASADENA. Tim Bartels of the U.K. Dementia Research Institute at University College, London, was encouraged by what the positive signals on secondary measures might mean for antibody development. “The results are very promising, and I think there is huge potential for improving [them],” he wrote. Bartels believes researchers may be able to refine the antibodies they use, based on ongoing investigations into what forms of α-synuclein are the most toxic in human brain. To Tiago Outeiro of University Medical Center Göttingen in Germany, the negative findings on primary imply that either prasinezumab did not target the correct toxic species, or that α-synuclein is not central to PD pathogenesis. “Future studies will be important to further document the actual effect of the antibody,” he wrote (full comment below).
What about other antibodies? In February, Biogen announced the discontinuation of cinpanemab development (see industry news). This antibody targeted α-synuclein’s N-terminus. Some preclinical data suggest that antibodies targeting the C-terminus, as prasinezumab does, may prove more effective (Masliah et al., 2005; Masliah et al., 2011; Games et al., 2014).
This may soon be tested, as other C-terminal-targeting antibodies are in the works. AstraZeneca’s MEDI1341 is in Phase 1, and Lundbeck’s LuAF82422 in Phase 1b. AbbVie had an α-synuclein antibody in Phase 1, ABBV-0805, but stopped the trial and has not announced future plans. The antibody is still listed in their pipeline. Meanwhile, UCB has just started Phase 1 with its α-synuclein antibody UCB7853.
Beyond antibodies, other PD drugs are in trials, targeting diverse pathogenic pathways (Apr 2018 conference news; Apr 2020 conference news). “The number of drugs in development has never been as large in the history of Parkinson’s,” Poewe noted at AD/PD.—Madolyn Bowman Rogers
References
Therapeutics Citations
News Citations
- α-Synuclein Antibody Appears Safe, Reaches Brain
- α-Synuclein Antibody Misses Primary, May Have Signal on Secondaries
- Do Smartphones Collect Better Clinical Data Than Paper-and-Pencil Tests?
- Parkinson’s Treatments Go After Genetic Targets
- Parkinson's Therapies Seek to Stem Progression
Paper Citations
- Masliah E, Rockenstein E, Adame A, Alford M, Crews L, Hashimoto M, Seubert P, Lee M, Goldstein J, Chilcote T, Games D, Schenk D. Effects of alpha-synuclein immunization in a mouse model of Parkinson's disease. Neuron. 2005 Jun 16;46(6):857-68. PubMed.
- Masliah E, Rockenstein E, Mante M, Crews L, Spencer B, Adame A, Patrick C, Trejo M, Ubhi K, Rohn TT, Mueller-Steiner S, Seubert P, Barbour R, McConlogue L, Buttini M, Games D, Schenk D. Passive immunization reduces behavioral and neuropathological deficits in an alpha-synuclein transgenic model of Lewy body disease. PLoS One. 2011 Apr 29;6(4):e19338. PubMed. RETRACTED
- Games D, Valera E, Spencer B, Rockenstein E, Mante M, Adame A, Patrick C, Ubhi K, Nuber S, Sacayon P, Zago W, Seubert P, Barbour R, Schenk D, Masliah E. Reducing C-terminal-truncated alpha-synuclein by immunotherapy attenuates neurodegeneration and propagation in Parkinson's disease-like models. J Neurosci. 2014 Jul 9;34(28):9441-54. PubMed.
External Citations
Further Reading
Annotate
To make an annotation you must Login or Register.

Comments
University Medical Center Goettingen
While the outcome of the trial is disappointing, the study was very important, as it tested an important hypothesis in the field—whether targeting α-synuclein using immunotherapy would be beneficial in PD. This is important because α-synuclein pathology is thought to play a major role in pathogenesis.
The fact that the primary outcome was not met can mean different things: either that α-synuclein pathology is not so central in pathogenesis, which would be important to know anyway, or that the trial did not target the toxic α-synuclein species, and that other antibodies may be necessary. This we will need to continue to investigate.
However, the trial showed that the antibody may reduce the decline in motor function, which, if correct, is still a major advance. So future studies will be important to further document the actual effect of the antibody and will, in any case, provide important information.
U.K. Dementia Research Institute at University College London
The results are very promising. I think that, in general, there is huge potential for improving the initial results, not only in terms of modifying the protocol but also in modifying the antibodies that are mostly developed against synthetic aggregate structures. How these compare to human brain-derived amyloid is under intense investigation, and we have more and more data coming in that will vastly improve the antibody development.
Furthermore, biomarkers will be key here, especially anything that will catch prodromal disease.
Targeting α-synuclein, which seems to be far upstream of the pathomechanism cascade, will be far more effective if done during the early stages of the disease.
Make a Comment
To make a comment you must login or register.