Cellular Alchemy: Turning Astroglia Into Neurons
Quick Links
Like alchemists aiming to turn base metals into gold, scientists are striving to convert one cell type into another—with a little more success. In a PLoS Biology paper posted May 18, researchers from the Ludwig-Maximilians University of Munich, Germany, report that they converted astroglia into neurons with the addition of just a single transcription factor. Moreover, they were able to make two kinds of neurons—excitatory glutamatergic neurons and inhibitory GABAergic neurons—by using different transcription factors. Leading the study were first author Christophe Heinrich and senior authors Magdalena Götz and Benedikt Berninger. The researchers hope that their work might eventually lead to new treatments for Alzheimer disease or stroke, Berninger said, although the current work is a very early step.
The researchers used radial glial cells as neural precursors. These cells exhibit long processes and express glial markers. Radial glia can become astrocytes or neurons during early development (Malatesta et al., 2000 and Noctor et al., 2001), but not in the adult cerebral cortex. “They have lost this ability,” Berninger said. The researchers forced them to reacquire it. Choosing radial glia probably gave the authors a head start, said Arnold Kriegstein of the University of California in San Francisco, who was not involved in the study. Radial glia “are not adult astrocytes,” he said. “They are probably just one step removed from neural stem cells.”
Götz and colleagues previously showed that neural transcription factors can induce certain types of glia to assume neural morphology (Heins et al., 2002), express early neuronal markers (Buffo et al., 2005), and fire action potentials (Berninger et al., 2007). However, getting the cells to make synaptic connections eluded the researchers.
Berninger and colleagues reasoned that higher levels of their chosen transcription factor, neurogenin-2 (Neurog2), might drive cells further toward the neural development pathway. So they cranked it up a notch with a stronger promoter. Previously, the researchers relied on the long terminal repeat-driven Moloney Monkey Leukemia Virus system, which is prone to silencing. This time around, they chose the chicken β-actin promoter (pCAG), which provides high-level transcription in the brain.
Heinrich and colleagues collected cerebral cortex cells from young mice (five to seven days old) and infected them with a virus containing the pCAG-Neurog2 construct. Then, they looked for the morphology and markers that would indicate neural differentiation. Just 10 days later, 70 percent of infected cells had shed the glial marker GFAP and acquired the neural protein βIII tubulin. Some also expressed Tbr1 and Tbr2, characteristic of glutamatergic neurons. After a few weeks, the transduced cells expressed MAP2 and demonstrated dendrite maturation.
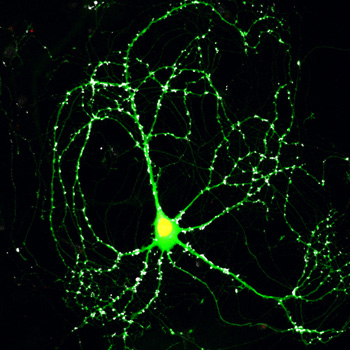
Did the new cells form synapses? Before checking via electrophysiology, the researchers looked for evidence of synapses with immunocytochemistry. They stained their cultures for the vesicular glutamate transporter 1 (vGluT1), a presynaptic component of glutamatergic neurons. Under the microscope, newly made dendrites were decorated with vGluT1, suggesting pre- and post-synaptic sites are in close proximity And by one month after Neurog2 expression, dendrites also contained the calmodulin-dependent kinase subunit IIα (CamKIIα), which is involved in synaptic plasticity and long-term potentiation—evidence for synapse activity (see image below).
Turning Astroglia Into Neurons
With a little neurogenin-2 (yellow), this cell that was once an astrocyte is now a neuron, complete with CamKII (green) and the synaptic marker vGluT1 (white). Image credit: Benedikt Berninger, Ludwig-Maximilians University
They look like synapses, yes, but do they function like synapses? To tackle this question, Götz and colleagues hooked up electrodes to examine the nerves’ activity. Depolarizing one neuron caused an electric current not only in that cell—an action potential—but also in nearby neurons, indicating the cells made functional synapses.
Neurog2 is associated with excitatory, glutamatergic neurons, and the researchers wondered if they had created this specific kind of nerve. When they treated their cultures with a glutamate receptor blocker, they abolished the currents. Neurog2-transduced cells also had no evidence of GABAergic connections, suggesting they had clearly moved towards an excitatory, not inhibitory, fate.
Having succeeded with excitatory neurons, the researchers attempted to produce their inhibitory counterparts, transducing astroglia with Dlx2, a key transcription factor in GABAergic neuron development. They achieved expression of βIII tubulin and MAP2 in 36 percent of transduced cells within 11 days. As desired, these cells had no vGluT but one-third evinced puncta that stained positive for vesicular GABA transporter (vGaT). In electrophysiology experiments, the neurons propagated synaptic signals, but the signals were typical of immature neurons, not full-fledged inhibitory nerves. The scientists suspect the complete maturation process is hampered in some way.
The researchers proved they can make more than one kind of neuron. “Maybe we could also make, if we choose the right factors, dopaminergic neurons or cholinergic neurons,” Berninger speculated; he is collaborating with other research groups to do just that.
However, the researchers weren’t fully satisfied with their recipe. Using viral transduction means that cells must divide in order to incorporate the new DNA, limiting the pool of changeable cells to those that undergo the cell cycle. Heinrich and colleagues wondered if cell division is necessary for the Neurog2 reprogramming process. They switched to transfection—no cell cycle required—and followed cells by time-lapse microscopy. They saw similar rates of neuron differentiation as in the transduction protocol, with 14 out of 17 transfected cells achieving neural morphology.
These results are all well and good for astroglia from very young mice, but what about adult animals? “To cure some patients, you would like to do this with more mature cells,” Berninger said. From previous work, the scientists knew that brain injury causes the proliferation of reactive astroglia (Buffo et al., 2008). In vitro, these cells can form neurospheres, balls of dividing, multipotent neural progenitors. “They make neurons, but they make very few,” Berninger said. He and his colleagues sought to improve that rate and control the neural fate, collecting astroglia from adult mice with brain lesions that produced neurospheres. Using Neurog2, they turned some of the neurosphere cells into glutamatergic neurons.
The astrocytes likely dedifferentiated as they formed neurospheres, then redifferentiated into neurons upon introduction of the transcription factors, the authors write. “It is not exactly turning adult astrocytes into nerve cells,” Kriegstein said. “But it is getting closer.”
The ultimate goal, Berninger said, is to force astrocytes to dedifferentiate and redifferentiate into neurons in the brain, without making a lesion or culturing the cells. If the scientists succeed, they might develop a treatment for stroke, epilepsy, or neurodegenerative diseases based on drugs or biologics that induce this transition in the brain. That might be easier and less invasive than other proposed treatment approaches that rely on cells that are differentiated in vitro, then transplanted into the brain. Doctors have had limited success with transplants for Parkinson disease, Berninger noted, but in that case only one cell type is missing, and only in one small specific area of the brain (see ARF related news story). In more complicated conditions, such as Alzheimer’s, it may not be possible to replace all the lost neurons. A protocol that relies on resident astroglia to fill in the blanks might be more successful.
The research is nowhere near that point yet, of course. “At least it tells us that, in principle, it must be possible,” Berninger said. For now, Berninger and colleagues are trying to achieve the astroglia-to-neuron transition in vivo.—Amber Dance.
Reference:
Heinrich C, Blum R, Gascón S, Masserdotti G, Tripathi P, Sánchez R, Tiedt S, Schroeder T, Götz M, Berninger B. Directing astroglia from the cerebral cortex into subtype specific functional neurons. PLoS Biol. 2010;8(5):e1000373. Abstract
References
News Citations
Paper Citations
- Malatesta P, Hartfuss E, Götz M. Isolation of radial glial cells by fluorescent-activated cell sorting reveals a neuronal lineage. Development. 2000 Dec;127(24):5253-63. PubMed.
- Noctor SC, Flint AC, Weissman TA, Dammerman RS, Kriegstein AR. Neurons derived from radial glial cells establish radial units in neocortex. Nature. 2001 Feb 8;409(6821):714-20. PubMed.
- Heins N, Malatesta P, Cecconi F, Nakafuku M, Tucker KL, Hack MA, Chapouton P, Barde YA, Götz M. Glial cells generate neurons: the role of the transcription factor Pax6. Nat Neurosci. 2002 Apr;5(4):308-15. PubMed.
- Buffo A, Vosko MR, Ertürk D, Hamann GF, Jucker M, Rowitch D, Götz M. Expression pattern of the transcription factor Olig2 in response to brain injuries: implications for neuronal repair. Proc Natl Acad Sci U S A. 2005 Dec 13;102(50):18183-8. PubMed.
- Berninger B, Costa MR, Koch U, Schroeder T, Sutor B, Grothe B, Götz M. Functional properties of neurons derived from in vitro reprogrammed postnatal astroglia. J Neurosci. 2007 Aug 8;27(32):8654-64. PubMed.
- Moyer RF. Systematic patient-dose errors for 4- and 10-MeV microwave linear accelerators associated with rectangular collimator settings. Radiology. 1978 Dec;129(3):803-6. PubMed.
- Heinrich C, Blum R, Gascón S, Masserdotti G, Tripathi P, Sánchez R, Tiedt S, Schroeder T, Götz M, Berninger B. Directing astroglia from the cerebral cortex into subtype specific functional neurons. PLoS Biol. 2010 May;8(5):e1000373. PubMed.
Further Reading
Papers
- Vierbuchen T, Ostermeier A, Pang ZP, Kokubu Y, Südhof TC, Wernig M. Direct conversion of fibroblasts to functional neurons by defined factors. Nature. 2010 Feb 25;463(7284):1035-41. PubMed.
- Malatesta P, Hack MA, Hartfuss E, Kettenmann H, Klinkert W, Kirchhoff F, Götz M. Neuronal or glial progeny: regional differences in radial glia fate. Neuron. 2003 Mar 6;37(5):751-64. PubMed.
- Buffo A, Rolando C, Ceruti S. Astrocytes in the damaged brain: molecular and cellular insights into their reactive response and healing potential. Biochem Pharmacol. 2010 Jan 15;79(2):77-89. PubMed.
- Berninger B, Hack MA, Götz M. Neural stem cells: on where they hide, in which disguise, and how we may lure them out. Handb Exp Pharmacol. 2006;(174):319-60. PubMed.
News
- Research Brief: From Fibroblast to Neuron in One Easy Step
- Circuit Menders? Neurogenesis, Stem Cells Show Potential
- Rewriting Cellular Destiny: Science Magazine’s Breakthrough of 2008
- Newest Stem Cell Approaches Abandon Viruses, Tap Testes
- Without a Trace: iPS Cell Techniques Leave No Footprints
- Stem Cell Advance—A Safer, Inducible Pluripotent Cell?
- Dopaminergic Transplants—Stable But Prone to Parkinson’s?
Primary Papers
- Heinrich C, Blum R, Gascón S, Masserdotti G, Tripathi P, Sánchez R, Tiedt S, Schroeder T, Götz M, Berninger B. Directing astroglia from the cerebral cortex into subtype specific functional neurons. PLoS Biol. 2010 May;8(5):e1000373. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.