Gearing Up for Down’s Syndrome Clinical Trials
Quick Links
Part 2 of two. Click here for Part 1.
For years, researchers have been paving the way for Down’s syndrome treatment studies by carrying out longitudinal observation studies. These have identified imaging, fluid biomarker, and cognitive measures that could serve as selection or outcome measures. In parallel, clinicians have identified people with Down's who are willing to take part in trials. Hundreds are expected to join trial-ready cohorts this year. Encouraged by the completion of AC Immune’s Phase 1 trial of an anti-amyloid vaccine in people with Down’s (see Part 1), researchers hope to test several other anti-amyloid treatments in these cohorts within the next few years.
- Biomarker trajectories in Down’s resemble those in Alzheimer's.
- Longitudinal studies show promise for amyloid PET, plasma NfL.
- Trial-ready cohorts are assembling, trials to come.
“It is truly amazing how much work has happened in the last five years,” Michael Rafii, University of Southern California, Los Angeles, told Alzforum. Juan Fortea, Hospital of Sant Pau, Barcelona, Spain, agreed. “It is a very exciting time for DS research, which benefits from a dramatic increase in attention and funding,” he wrote.
Natural History Studies
Efforts to characterize clinical and biomarker changes during AD progression in people with DS have gained momentum (Rafii et al., 2021). At present, at least nine cohorts in six countries are collecting biomarker data (see sidebar). Six cohorts in the EU are part of the European Horizon 21 Consortium, which tracks AD biomarkers and cognitive changes in more than 1,000 Down’s syndrome volunteers.
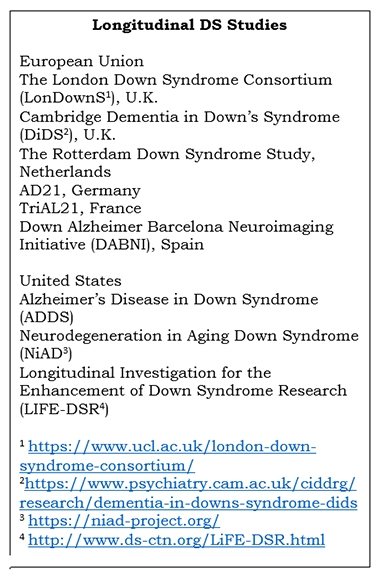
In the U.S., The Alzheimer’s Disease in Down Syndrome (ADDS) and Neurodegeneration in Aging Down Syndrome (NiAD) cohorts recently merged to create the National Institute on Aging’s Alzheimer's Biomarkers Consortium–Down Syndrome (ABC-DS) (Handen et al., 2020). In this cohort, scientists have collected imaging, fluid, and cognitive biomarkers from more than 400 people with DS age 25 and older. “The planned enrollment is just over 700, and there is a particular focus on increasing diversity,” Laurie Ryan, NIA, Bethesda, Maryland, told Alzforum. The scientists will compare how AD biomarkers change in DS relative to sporadic AD, search for genes that modify AD risk in DS, and apply what they learn to precision medicine approaches and clinical trials.
Also in the U.S., the LIFE-DSR natural history study aims to follow 270 people with DS aged 25 and older for 32 months, measuring plasma AD biomarkers, cognition, and behavior. It recruits using the U.S. Down Syndrome Clinical Trials Network (DS-CTN), which includes 11 clinic sites in nine states.
Biomarkers: Similar in Alzheimer’s and Down’s
What have researchers learned so far about how biomarkers change in Down's?
Markers begin shifting in a similar way, but at a much earlier age than in AD. In one cross-sectional study, Fortea and colleagues correlated memory, imaging, and fluid biomarker measures with age in 388 people with DS from the DABNI and DiDS cohorts (Fortea et al., 2020). They found that cerebrospinal fluid Aβ42/40 ratios fell and plasma neurofilament light (NfL) concentrations crept up in people’s 20s. Amyloid PET ligand uptake and CSF phospho-tau181 (p-tau181) began rising, while brain glucose metabolism started waning, by the 30s. The hippocampus atrophied and memory declined in people’s 40s. All this culminated in an AD diagnosis at an average age of 54.
In short, Fortea found almost identical AD biomarker trajectories in DS as did researchers led by Randall Bateman, Washington University, St. Louis, in autosomal-dominant AD (see image below and Bateman et al., 2012). “There is nothing to suggest that AD is categorically different in DS than in the general population,” Bradley Christian, University of Wisconsin, Madison, told Alzforum.
Likewise, researchers led by Dominic Walsh, then at Harvard Medical School, saw plasma Aβ42 fall, NfL rise, and the N-terminal tau fragment NT1 fall, then rise, in people with DS as they aged. Change was fastest in the 20s to 40s (Mengel et al., 2020).

Striking Similarity. Biomarkers and memory decline track similarly in familial AD (left) and DS (right). Most begin to change 15 to 20 years before age of symptom onset (dashed vertical line). For CDR-SOB and Cambridge Cognitive Examination–Down Syndrome (CAMCOG-DS), higher and lower scores, respectively, indicate worsening. CAMCOG-DS measures seven cognitive domains: orientation, language understanding and production, memory, attention, praxis, abstraction, and visual construction. [Courtesy of Bateman et al., NEJM, 2012 (left), and Fortea et al., Lancet, 2020.]
Tracking Plaques and Tangles
How can this biomarker information be used in clinical trials of DS?
In the case of Aβ, the data suggest it might help select the right candidates for trials. Christian and colleagues grouped people from the ABC-DS cohort by how fast their PET amyloid load changed (Zammit et al., 2021). Three groups emerged: “Aβ-negatives,” “Aβ-positives,” and a group deemed “converters” (see image below). Negatives had a low plaque load at baseline, which grew slowly. Positives had a high baseline plaque load, which grew quickly. Converters had a negative scan at baseline but accumulated plaques as fast as did positives.

All About Speed. People with DS, grouped by how fast plaques deposit in their brains over two to four measurement time points. [Courtesy of Zammit et al., NeuroImage, 2021.]
Christian proposed that lowering the amyloid-positivity threshold might catch some of the converters, and thus identify a group of people with DS who are at the earliest point of amyloid accumulation, irrespective of their age. He believes this might be a good group to test in trials of anti-amyloid therapies.
Similarly, scientists led by Ira Lott, University of California, Irvine, have identified a pattern of plaque accumulation that might indicate imminent dementia in DS. They took five PET scans over four years in 19 DS adults 40 years old or older without dementia at baseline. In five volunteers who developed dementia during the study, plaques built up in the same brain regions that typically accumulate amyloid in AD, including the inferior parietal cortex and temporal lobes. Buildup in the prefrontal and superior frontal cortices and posterior cingulate best predicted transition to dementia (Keator et al., 2020).
Focusing on change in specific regions of the brain might offer a way to reduce the length of time needed to see a treatment response in trials. Using PET data from 80 DS volunteers and 98 cognitively normal controls, researchers led by Ann Cohen at the University of Pittsburgh calculated that amyloid accumulated much faster in the striatum in DS than controls (Tudorascu et al., 2019).

Down’s Batwing. As tau spreads from the medial temporal lobe into the neocortex, a batwing pattern of tau tracer uptake appears. [Courtesy of Michael Rafii, ATRI and UCSD.]
Tau PET could hand DS researchers another trial measure. As in AD, scientists attribute the brain atrophy and memory problems in DS to neurofibrillary tangles. In a pilot study of 12 people with DS, three plaque-negative people had no neurofibrillary tangles, while the nine who did have plaques also had the characteristic “batwing” distribution of tangles (see image above). This shape appears as the tangles spread from the medial temporal lobe to the edges of, then throughout, the neocortex (Dec 2016 conference news). DS adults with AD also tend to accumulate more tangles in the medial frontal gyrus than do people with sporadic AD (Lemoine et al., 2020).
In DS, tangle burden correlated with atrophy on MRI, glucose hypometabolism measured by FDG PET, and cognitive decline (Rafii et al., 2017). In a study of 135 people with DS, of whom 11 had dementia, eight had mild cognitive impairment, 108 had no dementia, and eight had an unclear diagnosis; tangle load also tracked with plaque burden (Tudorascu et al., 2020).
Fluid Biomarkers
CSF Aβ42, total tau, p-tau181, and NfL all predicted AD in DS with AUCs over 0.90 (Fortea et al., 2018). However, plasma biomarkers have been the focus of late because blood draws are easier to tolerate than lumbar punctures or neuroimaging.
At the 2021 Global Down Syndrome Forum, a webcast co-sponsored by AC Immune about the latest research on AD in DS, Fortea presented results from a longitudinal study tracking plasma biomarkers. Together with colleagues at the University of Kentucky, he recruited 236 adults with Down’s from the DABNI, LonDownS, DiDS, TriAL21, and AD21 cohorts. He reported that people with high plasma NfL levels progressed to dementia faster than those with low blood NfL. In people who had advanced to symptomatic AD, their NfL concentration continued to rise, as has been shown for familial and sporadic AD (Aug 2019 conference news).
Smaller studies, as well, have shown plasma NfL rises as memory falters when people with DS develop AD (Shinomoto et al., 2019; Rafii et al., 2019). Likewise, Andre Strydom, King’s College London, and colleagues saw plasma NfL tick up with age in 100 Down's participants from the LonDownS cohort (Strydom et al., 2018). It rose steeply after age 40, with high levels predicting dementia. “Plasma NfL could be a theragnostic biomarker in DS clinical trials,” Fortea said.
Can plasma markers spot people with DS who have dementia? Collaborating with Henrik Zetterberg and Kaj Blennow at the University of Gothenburg, Sweden, and with Alberto Lleó at Hospital of Sant Pau, Fortea analyzed blood biomarkers in 366 DABNI volunteers and 44 controls. Plasma NfL and p-tau181 predicted AD in Down’s with AUCs of 0.96 and 0.92, respectively. P-tau181 also tracked closely with brain atrophy, and hypometabolism, and differentiated people who were Aβ-positive from those who weren't (Nov 2020 news).
Could combining plasma markers improve diagnosis? In 305 people with DS from the ABC-DS cohort, of whom 36 had AD and 44 had MCI, plasma NfL alone distinguished AD and MCI from controls with AUCs of 0.90 and 0.65, respectively, while for plasma total tau AUCs were 0.74 and 0.56, respectively (Petersen et al., 2021). When researchers combined the two biomarkers and accounted for age and gender, AUCs rose to 0.93 for AD and 0.87 for MCI.
Tracking Cognition
Ultimately, scientists want to correlate biomarker change with cognitive scores and clinical diagnoses so that they can have surrogate measures for clinical trial selection and monitoring. Alas, cognitive tests for DS have been tricky to develop. In recent years, though, researchers have made progress modifying AD tests such that they now can account for the wide range of intellectual disabilities seen in Down’s itself (Channell et al., 2021).
One such tool is the modified Cambridge Examination for Mental Disorders in the Elderly (CAMDEX-DS). It relies on the clinician’s judgement to diagnose dementia (Ball et al., 2004). Shahid Zaman, University of Cambridge, U.K., and colleagues established CAMDEX-DS cut-off scores for prodromal AD and AD in DS. The thresholds correlated tightly with psychiatrist diagnoses of prodromal AD and AD in DS adults who had no mental health conditions, but were less sensitive in people who did have such conditions (Beresford-Webb et al., 2021).
Modifying a different AD test, John Constantino at WashU and colleagues adapted the CDR scale to better stage dementia in DS. It captured a range of cognitive impairments among 34 people with DS recruited from the surrounding community in St Louis. It even detected deficits in half of those volunteers who had been deemed non-demented by the Dementia Scale for Down Syndrome test, suggesting this modified CDR may be a more sensitive test (Lessov-Schlaggar et al., 2019).
One way to improve diagnosis of dementia might be to divide people with DS into groups based on the severity of their intellectual disability. “That gives you a bit more power to predict AD, with less variability,” Zaman told Alzforum.

Inflection Points. Already in their 30s, people with DS experience a decline in visual memory (PAL), executive function (Tower of London), hand-eye coordination (finger-nose), and orientation. Immediate object memory and other measures of executive function—Intra-Extra Dimensional Shift Task (IED) and Behavior Rating Inventory of Executive Function (BRIEF)—follow in the 40s. Delayed object memory, memory noted by a caregiver (Observer Memory Questionnaire revised edition, OMQ-R), and sustained attention (SRT mean latency) falter in the 50s. [Courtesy of Hithersay et al., Alzheimer’s & Dementia, 2021.]
Another option for tracking dementia might be to focus on specific cognitive domains. Researchers led by Christian tracked cognition and plaque accumulation in 118 ABC-DS participants without dementia who were 25 and older. Decline in the Cued Recall Test (CRT), which measures episodic memory, tracked with plaques and predicted AD onset (Hartley et al., 2020).
In another study of 173 adults with DS ages 36 and older from the LonDownS cohort, Strydom and colleagues used statistical modeling to pinpoint when the decline of several cognitive domains speeds up (Hithersay et al., 2021). Memory, executive function, and hand-eye coordination faded first, followed by orientation, sustained attention, language abilities, and finally daily functioning (see image above). “Cognitive measures of memory and attention are useful as outcome measures during early stages, while functional measures are more useful during later stages,” Strydom said.
What to Use in Trials?
Which of these options are best suited to treatment trials? Rafii suggests amyloid PET as a primary measure, and rate of change in tau as measured by PET, atrophy measured by volumetric MRI, or FDG PET as secondary measures. Fortea agreed, writing that amyloid and tau PET will be required outcome measures for anti-amyloid and anti-tau therapies.
Plasma NfL and p-tau181 also stand out. “I think they will play a critical role in AD trials for patient selection, target engagement, and outcome measurement,” Fortea wrote. Again, William Mobley, University of California, San Diego, and Zaman agreed. “Plasma NfL and p-tau181 are going to be very useful for not only prognosis, but also indicating disease stage,” Zaman said. Lott remains cautious. “Many biomarker studies show a DS signature, but it is not yet clear whether, either singly or together, those signatures can predict the actual conversion to dementia,” he wrote to Alzforum.
Much as biomarkers look promising, Strydom noted that cognitive and functional measures are essential to diagnosing Down's dementia, tracking it, and measuring treatment effects in trials. “Ultimately, FDA approval may depend on clinical outcome measures and on the clinical meaningfulness of findings, rather than solely on biomarkers,” he wrote to Alzforum, echoing the experience Alzheimer's scientists made in the early years of biomarker development in that field.
What would those cognitive measures be? Strydom and colleagues recommend the Cambridge Neuropsychological Test Automated Battery Paired Associates Learning (CANTAB PAL), the CANTAB simple reaction time (SRT), and the Tower of London tests, which measure visual memory, attention, and executive function, respectively. These accurately detect subtle changes over two years in people with DS ages 35 to 40.
The CANTAB PAL can be taken on a tablet computer, making it easy to use in trials. However, it does not work for all stages. “It may be a good outcome measure to use during early stage AD, but it becomes increasingly difficult for people to perform as they progress into dementia,” Strydom said.
Strydom and colleagues have compared cognitive tests to identify a standardized battery for use in clinical trials. At the Global DS Forum, he showed how cognition changed over time in people with DS who had prodromal AD. The data came from volunteers at the University of Kentucky; University of Pittsburgh; University of Wisconsin, Madison; LonDownS; DiDS; and DABNI. The researchers identified six tests that could be used in the battery: on a modified CRT and CANTAB PAL to measure memory; verbal fluency tests for language ability; the Purdue Pegboard test for dexterity; a subset of the Cambridge Cognitive Examination–Down Syndrome (CAMCOG-DS) for orientation; and the Cancellation task for attention. The CANTAB SRT has not been incorporated into the company’s tablet platform, so Strydom is developing a similar digital test to take its place.
Cohorts Ready for Trials
Even as researchers reach consensus on what the best outcome measures may be, they are recruiting adults with DS who want to join AD prevention trials. As in AD itself, such trial-ready cohorts collect baseline biomarker and cognitive data so that participants are ready to enroll in a future clinical trial.
In Europe, Strydom and colleagues in the Horizon21 Consortium are coordinating participants from the six existing cohorts there (Strydom et al., 2018). The researchers will initially focus on collecting longitudinal plasma biomarker data and validating potential clinical outcome measures. Strydom said it was too early to say which markers and outcomes will be tracked. The hope is to roll this cohort into a treatment trial with clinical outcomes, such as cognition and symptom improvement. They plan for 240 participants, though recruitment remains suspended due to COVID.
Simultaneously, Rafii and colleagues at 12 different research centers in the U.S. and three in Europe are also assembling a trial-ready cohort. Called TRC-DS, it is based on the TRC-PAD cohort assembled for studying preclinical and prodromal AD (Nov 2020 conference news). It will engage at least 12 of the 35 Alzheimer’s Clinical Trials Consortium (ACTC) trial sites in the U.S. and Europe to run trials in Down's. This subset is dubbed ACTC-DS.
TRC-DS invites people with DS who are 35 to 55 years old, do not yet have dementia, and who want to participate in a clinical trial within the next few years. Enrollment of 120 volunteers is to start this month, and people in the ABC-DS observational cohort are eligible. “Hopefully TRC-DS will be fully enrolled by this summer, finish initial data collection by fall of 2022, and launch a clinical trial in late 2023,” Ryan said.
Echoing the process established for DIAN, a committee will review investigational anti-amyloid drugs and pick the most suitable for the first TRC-DS trial. For subsequent trials, the committee is eying anti-tau drugs and antisense oligonucleotides against APP. One candidate might be splice-switching oligonucleotides, which trick the splicing machinery into skipping the exon encoding Aβ, reducing Aβ production (Jun 2018 news).—Chelsea Weidman Burke
References
News Citations
- In Down's Syndrome, Amyloid Vaccine Opens Door to Trials
- Tau PET in Down’s: Unique Patterns Among Alzheimer’s Types and Stages
- Colombian Cohort Delivers Data on Blood NfL
- Plasma Aβ Test Wins Approval—Are p-Tau Tests Far Behind?
- TRC-PAD Funnel Finally Touches Down
- Antisense Oligonucleotides Turn Down the Aβ Spigot
Paper Citations
- Rafii MS, Zaman S, Handen BL. Integrating Biomarker Outcomes into Clinical Trials for Alzheimer's Disease in Down Syndrome. J Prev Alzheimers Dis. 2021;8(1):48-51. PubMed.
- Handen BL, Lott IT, Christian BT, Schupf N, OBryant S, Mapstone M, Fagan AM, Lee JH, Tudorascu D, Wang MC, Head E, Klunk W, Ances B, Lai F, Zaman S, Krinsky-McHale S, Brickman AM, Rosas HD, Cohen A, Andrews H, Hartley S, Silverman W, Alzheimer's Biomarker Consortium‐Down Syndrome (ABC‐DS). The Alzheimer's Biomarker Consortium-Down Syndrome: Rationale and methodology. Alzheimers Dement (Amst). 2020;12(1):e12065. Epub 2020 Aug 3 PubMed.
- Fortea J, Vilaplana E, Carmona-Iragui M, Benejam B, Videla L, Barroeta I, Fernández S, Altuna M, Pegueroles J, Montal V, Valldeneu S, Giménez S, González-Ortiz S, Muñoz L, Estellés T, Illán-Gala I, Belbin O, Camacho V, Wilson LR, Annus T, Osorio RS, Videla S, Lehmann S, Holland AJ, Alcolea D, Clarimón J, Zaman SH, Blesa R, Lleó A. Clinical and biomarker changes of Alzheimer's disease in adults with Down syndrome: a cross-sectional study. Lancet. 2020 Jun 27;395(10242):1988-1997. PubMed.
- Bateman RJ, Xiong C, Benzinger TL, Fagan AM, Goate A, Fox NC, Marcus DS, Cairns NJ, Xie X, Blazey TM, Holtzman DM, Santacruz A, Buckles V, Oliver A, Moulder K, Aisen PS, Ghetti B, Klunk WE, McDade E, Martins RN, Masters CL, Mayeux R, Ringman JM, Rossor MN, Schofield PR, Sperling RA, Salloway S, Morris JC. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N Engl J Med. 2012 Aug 30;367(9):795-804. PubMed.
- Mengel D, Liu W, Glynn RJ, Selkoe DJ, Strydom A, Lai F, Rosas HD, Torres A, Patsiogiannis V, Skotko B, Walsh DM. Dynamics of plasma biomarkers in Down syndrome: the relative levels of Aβ42 decrease with age, whereas NT1 tau and NfL increase. Alzheimers Res Ther. 2020 Mar 19;12(1):27. PubMed.
- Zammit MD, Tudorascu DL, Laymon CM, Hartley SL, Zaman SH, Ances BM, Johnson SC, Stone CK, Mathis CA, Klunk WE, Cohen AD, Handen BL, Christian BT. PET measurement of longitudinal amyloid load identifies the earliest stages of amyloid-beta accumulation during Alzheimer's disease progression in Down syndrome. Neuroimage. 2021 Mar;228:117728. Epub 2021 Jan 7 PubMed.
- Keator DB, Doran E, Taylor L, Phelan MJ, Hom C, Tseung K, van Erp TG, Potkin SG, Brickman AM, Rosas DH, Yassa MA, Silverman W, Lott IT. Brain amyloid and the transition to dementia in Down syndrome. Alzheimers Dement (Amst). 2020;12(1):e12126. Epub 2020 Nov 11 PubMed.
- Tudorascu DL, Anderson SJ, Minhas DS, Yu Z, Comer D, Lao P, Hartley S, Laymon CM, Snitz BE, Lopresti BJ, Johnson S, Price JC, Mathis CA, Aizenstein HJ, Klunk WE, Handen BL, Christian BT, Cohen AD. Comparison of longitudinal Aβ in nondemented elderly and Down syndrome. Neurobiol Aging. 2019 Jan;73:171-176. Epub 2018 Sep 27 PubMed.
- Lemoine L, Ledreux A, Mufson EJ, Perez SE, Simic G, Doran E, Lott I, Carroll S, Bharani K, Thomas S, Gilmore A, Hamlett ED, Nordberg A, Granholm AC. Regional binding of tau and amyloid PET tracers in Down syndrome autopsy brain tissue. Mol Neurodegener. 2020 Nov 23;15(1):68. PubMed.
- Rafii MS, Lukic AS, Andrews RD, Brewer J, Rissman RA, Strother SC, Wernick MN, Pennington C, Mobley WC, Ness S, Matthews DC, Down Syndrome Biomarker Initiative and the Alzheimer’s Disease Neuroimaging Initiative. PET Imaging of Tau Pathology and Relationship to Amyloid, Longitudinal MRI, and Cognitive Change in Down Syndrome: Results from the Down Syndrome Biomarker Initiative (DSBI). J Alzheimers Dis. 2017;60(2):439-450. PubMed.
- Tudorascu DL, Laymon CM, Zammit M, Minhas DS, Anderson SJ, Ellison PA, Zaman S, Ances BM, Sabbagh M, Johnson SC, Mathis CA, Klunk WE, Handen BL, Christian BT, Cohen AD. Relationship of amyloid beta and neurofibrillary tau deposition in Neurodegeneration in Aging Down Syndrome (NiAD) study at baseline. Alzheimers Dement (N Y). 2020;6(1):e12096. Epub 2020 Oct 31 PubMed. Correction.
- Fortea J, Carmona-Iragui M, Benejam B, Fernández S, Videla L, Barroeta I, Alcolea D, Pegueroles J, Muñoz L, Belbin O, de Leon MJ, Maceski AM, Hirtz C, Clarimón J, Videla S, Delaby C, Lehmann S, Blesa R, Lleó A. Plasma and CSF biomarkers for the diagnosis of Alzheimer's disease in adults with Down syndrome: a cross-sectional study. Lancet Neurol. 2018 Oct;17(10):860-869. Epub 2018 Aug 29 PubMed.
- Shinomoto M, Kasai T, Tatebe H, Kondo M, Ohmichi T, Morimoto M, Chiyonobu T, Terada N, Allsop D, Yokota I, Mizuno T, Tokuda T. Plasma neurofilament light chain: A potential prognostic biomarker of dementia in adult Down syndrome patients. PLoS One. 2019;14(4):e0211575. Epub 2019 Apr 5 PubMed.
- Rafii MS, Donohue MC, Matthews DC, Muranevici G, Ness S, O'Bryant SE, Rissman RA. Plasma Neurofilament Light and Alzheimer's Disease Biomarkers in Down Syndrome: Results from the Down Syndrome Biomarker Initiative (DSBI). J Alzheimers Dis. 2019;70(1):131-138. PubMed.
- Strydom A, Heslegrave A, Startin CM, Mok KY, Hardy J, Groet J, Nizetic D, Zetterberg H, LonDownS Consortium. Neurofilament light as a blood biomarker for neurodegeneration in Down syndrome. Alzheimers Res Ther. 2018 Apr 10;10(1):39. PubMed.
- Petersen ME, Rafii MS, Zhang F, Hall J, Julovich D, Ances BM, Schupf N, Krinsky-McHale SJ, Mapstone M, Silverman W, Lott I, Klunk W, Head E, Christian B, Foroud T, Lai F, Diana Rosas H, Zaman S, Wang MC, Tycko B, Lee JH, Handen B, Hartley S, Fortea J, O'Bryant S, Alzheimer’s Biomarker Consortium –Down Syndrome (ABC-DS). Plasma Total-Tau and Neurofilament Light Chain as Diagnostic Biomarkers of Alzheimer's Disease Dementia and Mild Cognitive Impairment in Adults with Down Syndrome. J Alzheimers Dis. 2021;79(2):671-681. PubMed.
- Channell MM, Mattie LJ, Hamilton DR, Capone GT, Mahone EM, Sherman SL, Rosser TC, Reeves RH, Kalb LG, Down Syndrome Cognition Project. Capturing cognitive and behavioral variability among individuals with Down syndrome: a latent profile analysis. J Neurodev Disord. 2021 Apr 19;13(1):16. PubMed.
- Ball SL, Holland AJ, Huppert FA, Treppner P, Watson P, Hon J. The modified CAMDEX informant interview is a valid and reliable tool for use in the diagnosis of dementia in adults with Down's syndrome. J Intellect Disabil Res. 2004 Sep;48(Pt 6):611-20. PubMed.
- Beresford-Webb JA, Mak E, Grigorova M, Daffern SJ, Holland AJ, Zaman SH. Establishing diagnostic thresholds for Alzheimer's disease in adults with Down syndrome: the Cambridge Examination for Mental Disorders of Older People with Down's Syndrome and Others with Intellectual Disabilities (CAMDEX-DS). BJPsych Open. 2021 Apr 13;7(3):e79. PubMed.
- Lessov-Schlaggar CN, Del Rosario OL, Morris JC, Ances BM, Schlaggar BL, Constantino JN. Adaptation of the Clinical Dementia Rating Scale for adults with Down syndrome. J Neurodev Disord. 2019 Dec 16;11(1):39. PubMed.
- Hartley SL, Handen BL, Devenny D, Tudorascu D, Piro-Gambetti B, Zammit MD, Laymon CM, Klunk WE, Zaman S, Cohen A, Christian BT. Cognitive indicators of transition to preclinical and prodromal stages of Alzheimer's disease in Down syndrome. Alzheimers Dement (Amst). 2020;12(1):e12096. Epub 2020 Sep 13 PubMed.
- Hithersay R, Baksh RA, Startin CM, Wijeratne P, Hamburg S, Carter B, LonDownS Consortium, Strydom A. Optimal age and outcome measures for Alzheimer's disease prevention trials in people with Down syndrome. Alzheimers Dement. 2021 Apr;17(4):595-604. Epub 2020 Nov 23 PubMed.
- Strydom A, Coppus A, Blesa R, Danek A, Fortea J, Hardy J, Levin J, Nuebling G, Rebillat AS, Ritchie C, van Duijn C, Zaman S, Zetterberg H. Alzheimer's disease in Down syndrome: An overlooked population for prevention trials. Alzheimers Dement (N Y). 2018;4:703-713. Epub 2018 Dec 13 PubMed.
External Citations
Further Reading
Papers
- Krinsky-McHale SJ, Zigman WB, Lee JH, Schupf N, Pang D, Listwan T, Kovacs C, Silverman W. Promising outcome measures of early Alzheimer's dementia in adults with Down syndrome. Alzheimers Dement (Amst). 2020;12(1):e12044. Epub 2020 Jul 5 PubMed.
- Petersen ME, Zhang F, Schupf N, Krinsky-McHale SJ, Hall J, Mapstone M, Cheema A, Silverman W, Lott I, Rafii MS, Handen B, Klunk W, Head E, Christian B, Foroud T, Lai F, Rosas HD, Zaman S, Ances BM, Wang MC, Tycko B, Lee JH, O'Bryant S, Alzheimer's Biomarker Consortium – Down Syndrome (ABC‐DS). Proteomic profiles for Alzheimer's disease and mild cognitive impairment among adults with Down syndrome spanning serum and plasma: An Alzheimer's Biomarker Consortium-Down Syndrome (ABC-DS) study. Alzheimers Dement (Amst). 2020;12(1):e12039. Epub 2020 Jun 30 PubMed.
- Snyder HM, Bain LJ, Brickman AM, Carrillo MC, Esbensen AJ, Espinosa JM, Fernandez F, Fortea J, Hartley SL, Head E, Hendrix J, Kishnani PS, Lai F, Lao P, Lemere C, Mobley W, Mufson EJ, Potter H, Zaman SH, Granholm AC, Rosas HD, Strydom A, Whitten MS, Rafii MS. Further understanding the connection between Alzheimer's disease and Down syndrome. Alzheimers Dement. 2020 Jul;16(7):1065-1077. Epub 2020 Jun 16 PubMed.
- Handen BL. The Search for Biomarkers of Alzheimer's Disease in Down Syndrome. Am J Intellect Dev Disabil. 2020 Mar;125(2):97-99. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.