Do Gene Expression Signatures of Aging Signal AD?
Quick Links
Aging is a prerequisite for late-onset AD, but how does the aging process lead to AD in some people, but not others? Wielding gene expression data from multiple datasets to address this question, researchers led by Zhidong Tu at the Icahn School of Medicine at Mount Sinai, New York, report similarities and differences between gene expression signatures in healthy aging brains versus those wracked with AD.
In the hippocampus, energy metabolism and synaptic function wane with normal aging and in AD, while neuroinflammation rages more in the latter. The researchers found that not all brain transcriptomes age equally. An AD-like gene expression signature emerged in a subset of cognitively normal people who died between the ages of 45 and 70. The findings suggest that, in some, the brain aging process veers toward AD many years prior to the typical onset of the disease. They also raise the possibility that by middle age, biomarkers of aging might predict future disease in time to prevent it.
- Postmortem transcriptomics of aging and AD compared.
- Both suggest loss of synaptic and metabolic dysfunction.
- Immune and inflammatory genes rev up more in AD.
- Transcriptomes of some healthy people under 70 resembled that of AD.
Past studies have compared gene expression changes that occur with age to those that crop up in people with AD (Berchtold et al., 2013; Lanke et al., 2018). However, it has long been unclear whether the pattern of brain aging in those destined to develop AD differs from those who will remain sharp into old age. Definitively answering that question with postmortem data is technically not feasible. Still, first author Shouneng Peng and colleagues integrated multiple postmortem datasets, and clever computational analyses, to get at the question in a cross-sectional study.
First, the authors identified gene expression signatures associated with age. To do this, Peng compared expression patterns in different brain regions from the Genotype-Tissue Expression (GTEx) and UK Brain Expression Consortium (UKBEC) datasets. Collectively, samples from these two datasets came from donors between the ages of 20 and 70 who were free of any sign of neurological disorders at death, including amyloid and tau pathology. Aging signatures emerged from 11 of 13 brain regions sampled in GTEx, and from eight of 10 brain regions sampled in UKBEC. Next, Peng compared these aging signatures with AD gene expression signatures derived from multiple other cohorts, including Mount Sinai School of Medicine, the Mayo Clinic Brain Bank, and the Religious Orders Study and Memory and Aging Project (ROSMAP) (Wang et al., 2016; Jun 2018 news; Annese et al., 2018; van Rooij et al., 2019).
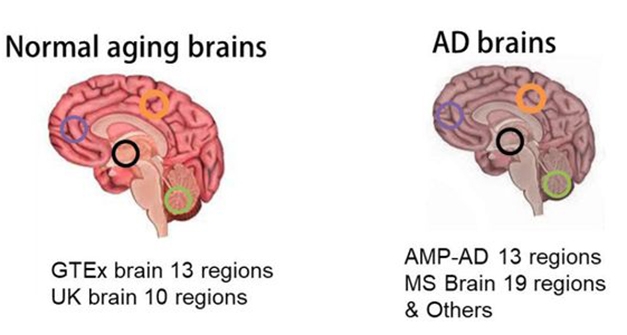
Aging Versus AD. Gene expression signatures of aging were derived from brain samples in the GTEx and UKBEC datasets, while AD signatures came from previously published finds from the Mayo Clinic, Mount Sinai, ROSMAP, and others. [Courtesy of Peng et al., bioRxiv, 2021.]
In all, the scientists pulled out 91 aging genes—27 upregulated and 64 downregulated with age—and 86 AD genes, among which 51 were dialed up and 35 turned down in people with AD across several of the cohorts. In short, both the aging and AD signatures suggested an uptick in immune response genes, and a dialing down of synaptic function. For example, expression of the gene encoding synaptic vesicle 2 related protein (SVOP), a protein involved in synaptic vesicle transport, was consistently dialed down in both aging and AD signatures, as was expression of somatostatin (SST), a neuropeptide hormone that maintains the blood-brain barrier.
The scientists next broke down the aging and AD signatures by brain region. Interestingly, they identified distinct signatures of aging in different areas of the brain, with the hypothalamus, hippocampus, and cortex affected the most by aging, at least at the transcriptome level. AD signatures in each region largely overlapped with the age-related changes specific to that region.
Moving forward, Peng and colleagues focused in on the hippocampus, an area of the brain highly affected by both aging and AD. Here again they found that while erosion of fundamental processes such as transcriptional regulation, energy metabolism, membrane remodeling, and synaptic function were implied by both aging and AD signatures, other functions, particularly inflammation and immune responses, changed more markedly in people with AD.
Given the similarities between aging and AD gene expression profiles, why do only some people develop AD? The researchers hypothesized that this could be explained by different types of aging—some of which may align more tightly with the disease. To test this, they took a closer look at the hippocampal aging signatures in the cognitively normal people between the ages of 45 and 70 in the GTEx and UK cohorts. They identified three transcriptional subgroups, each with a different aging signature. Strikingly, two subgroups—defined as “AD-similar”—were more closely aligned with the AD signature than the other subgroup, dubbed “healthy aging.”

Aging Toward AD? Three age-related gene expression signatures emerged in the hippocampus among cognitively normal people who died between 45 and 70 years of age. The researchers compared each aging signature to the AD signature in an older cohort (right). Two aging signatures, B and C, resembled the AD signature. [Courtesy of Peng et al., bioRXiv, 2021.]
Had they lived into their 70s, would people with an “AD similar” gene profile in their hippocampus have been more likely to develop AD? There is no direct way to answer that question, so the researchers took an indirect approach. They compared the AD-similar and healthy aging gene signatures gleaned from the GTEx and UKBEC cohorts to gene expression profiles in another cohort of people older than 70. Derived from Mount Sinai, this separate cohort comprised parahippocampal gyrus brain samples from 19 people who were deemed cognitively normal and free of amyloid or tau pathology at death, and 59 others who had had both clinical and neuropathological evidence of AD. Donors ranged from 70 to 104 years old. Lo and behold, the gene expression of the cognitively normal people in the older Mount Sinai cohort “aligned with that of the healthy aging” subgroup from the younger GTEx/UKBEC cohort, while the gene expression profile of the people with AD in the older Mount Sinai cohort aligned with the “AD similar” subgroup in the GTEx/UKBEC samples. Together, this suggested that sometime in middle age, the brain starts to age in a way that charts the course to either AD or cognitive resilience in older age.
Tu believes that collectively, the data suggest that with aging comes deterioration of basic biological functions critical to maintaining cellular health, which may occur earlier in people who are on the path to AD. This cellular distress provokes inflammatory responses, which exacerbate destruction and ultimately lead to neurodegeneration.
To Jeroen van Rooij of Erasmus University in Rotterdam, studies like this could help distinguish between nonspecific changes and insults that occur with normal aging, and those that occur in specific disease states, including AD.
Tu plans to use the data to find aging biomarkers that could predict, in middle age, if a person is on the path to AD. “I hope this work can send a message that we really should spend more time looking at relatively early stage changes in aging that could potentially lead to development of AD,” he said.
Andrea Tenner of the University of California, Irvine, commented that the identification of different aging signatures, some of which appear to be AD-like, is useful. “Additional steps are needed to determine if those expression signatures are deterministic of the development of AD or the age of onset of AD, and/or what environmental factors synergize to induce the neuronal dysfunction that results in cognitive loss,” Tenner wrote. She wondered how these gene expression profiles correlate with the AD subtypes reported by several of the authors earlier this year (Jan 2021 news).
Commentators both praised and lamented the study’s integration of multiple datasets in its analysis, which makes the data challenging to interpret. Karl Herrup of the University of Pittsburgh in Pennsylvania noted that many of the genes that the authors included in the aging and AD signatures only changed expression in a minority of the datasets. “One of the things that I take away from the entire exercise is that both AD and aging, even in this fairly homogeneous cohort, are incredibly variable,” Herrup wrote.—Jessica Shugart
References
News Citations
- Culling Connection From Chaos, Alzheimer’s Genetic Network Study Pins PLXNB1 and INPPL1
- Expression Analysis Uncovers Three Distinct Forms of Alzheimer’s
Paper Citations
- Berchtold NC, Coleman PD, Cribbs DH, Rogers J, Gillen DL, Cotman CW. Synaptic genes are extensively downregulated across multiple brain regions in normal human aging and Alzheimer's disease. Neurobiol Aging. 2013 Jun;34(6):1653-61. PubMed.
- Lanke V, Moolamalla ST, Roy D, Vinod PK. Integrative Analysis of Hippocampus Gene Expression Profiles Identifies Network Alterations in Aging and Alzheimer's Disease. Front Aging Neurosci. 2018;10:153. Epub 2018 May 23 PubMed.
- Wang M, Roussos P, McKenzie A, Zhou X, Kajiwara Y, Brennand KJ, De Luca GC, Crary JF, Casaccia P, Buxbaum JD, Ehrlich M, Gandy S, Goate A, Katsel P, Schadt E, Haroutunian V, Zhang B. Integrative network analysis of nineteen brain regions identifies molecular signatures and networks underlying selective regional vulnerability to Alzheimer's disease. Genome Med. 2016 Nov 1;8(1):104. PubMed.
- Annese A, Manzari C, Lionetti C, Picardi E, Horner DS, Chiara M, Caratozzolo MF, Tullo A, Fosso B, Pesole G, D'Erchia AM. Whole transcriptome profiling of Late-Onset Alzheimer's Disease patients provides insights into the molecular changes involved in the disease. Sci Rep. 2018 Mar 9;8(1):4282. PubMed.
- van Rooij JG, Meeter LH, Melhem S, Nijholt DA, Wong TH, Netherlands Brain Bank, Rozemuller A, Uitterlinden AG, van Meurs JG, van Swieten JC. Hippocampal transcriptome profiling combined with protein-protein interaction analysis elucidates Alzheimer's disease pathways and genes. Neurobiol Aging. 2019 Feb;74:225-233. Epub 2018 Oct 29 PubMed.
Further Reading
No Available Further Reading
Primary Papers
- Peng S, Zeng L, Haure-Mirande JV, Wang M, Huffman DM, Haroutunian V, Erlich M, Zhang B, Tu Z. Transcriptomic changes highly similar to Alzheimer’s disease are observed in a subpopulation of individuals during normal brain aging. bioRxiv, July 13, 2021 bioRxiv.
Annotate
To make an annotation you must Login or Register.

Comments
University of California, Irvine
There are many useful findings in this study, such as differences in gene expression involving energy metabolism and synapse pathways as indicators of healthy aging vs. “escalated” inflammation/immune responses in AD, and the presence of “AD-like” gene expression signatures in subsets of young (40 to 70 years of age) individuals.
Additional steps are needed to determine if those expression signatures are deterministic of the development of AD, or the age of onset of AD, and/or what environmental factors synergize to induce the neuronal dysfunction that results in cognitive loss. In addition, it would be interesting to know how these gene expression profiles correlate with the AD subtypes reported by several of the authors earlier this year (Neff et al., 2021). …More
References:
Neff RA, Wang M, Vatansever S, Guo L, Ming C, Wang Q, Wang E, Horgusluoglu-Moloch E, Song WM, Li A, Castranio EL, Tcw J, Ho L, Goate A, Fossati V, Noggle S, Gandy S, Ehrlich ME, Katsel P, Schadt E, Cai D, Brennand KJ, Haroutunian V, Zhang B. Molecular subtyping of Alzheimer's disease using RNA sequencing data reveals novel mechanisms and targets. Sci Adv. 2021 Jan;7(2) Print 2021 Jan PubMed.
University of Pittsburgh School of Medicine
First and most important, kudos to the authors for taking on the project. It's a great concept and we end up with a really useful dataset that others can use to test ideas about AD ... and aging.
From the methodological point of view, I do have some reservations. The first is unavoidable. Our genetic resources are neither diverse nor representative. So their conclusions basically apply only to white Caucasian aging and AD. The second is more subtle. The brain regions sampled are not uniform across the CNS. It's quite interesting that the more "primitive" subcortical regions (like spinal cord) don't show a strong aging signature. But they are poorly represented in the AD cohorts. Also, the hypothalamus has my attention recently because of some lovely work on metabolism and aging by Suzana Herculano-Houzel. She identified it as a key to aging and according to Peng et al. it was the brain area with the most up-/downregulated genes of all. The problem is that it only appears in one of the aging sets (GTEx Aging) and none of the others. That is unfortunate and raises the question of whether their analysis compensated appropriately for the heterogeneity. (Also, why does no one seem to care about the amygdala?)…More
The analysis itself also makes me nervous. They look for genes that are consistently changed with age or disease. First of all, their criteria are pretty loose (change was required in only four of 19 datasets). Then they do pathway analysis of these genes. I get it, but I confess to be thinking here that the glass is half-empty (see variability comments below). I was pleased that they looked at specific regions to see if there were regional differences in aging/AD signatures. But it's not clear to me how valid the comparisons are if a brain region (for example, hypothalamus) is not in all of your datasets. And statistically valid does not always mean biologically meaningful.
Also, continuing in my role as crotchety curmudgeon, the global changes that they report don't tell us much that we didn't already know. Neuronal proteins go down; immune system proteins go up. A few items such as the insulin/lipid data are interesting, but not followed up. The single genes they cite could be interesting, but from what they've shown us we can't be sure.
One of the things that I take away from the entire exercise is that both AD and aging, even in this fairly homogeneous cohort, are incredibly variable. Figure 3 is a great example. Of all the genes in the four datasets graphed, only five upregulated and 15 downregulated genes were common to all four. By far the biggest numbers in the Venn diagrams are the single-color (one dataset) regions. The same can be said for the AD datasets. They focus their discussion on the more closely aligned GTX and UK datasets in their discussion, but to me the numbers still are not that impressive and excluding the others basically misses the point of the entire exercise. The other datasets should be like validation sets, but they don't seem to validate very strongly.
Erasmus Medical Centre
The authors extracted age signatures from healthy brain studies and compared them to disease signatures from AD case-control studies. They observed overlap between these signatures, and were able to cluster some cognitively healthy individuals based on their similarity with AD signatures.
As the authors suggest, this similarity probably indicates that these individuals were on the path toward a late-onset AD (LOAD) phenotype, and what we observe are the earlier stages thereof. This is in line with the idea that the disease begins long before the first clinical complaints, which also pans out in imaging or fluid biomarker studies. It is of interest that these healthy brains do not yet show the common pathological changes of AD, suggesting that these (milder?) regulation changes precede pathology. Of course, what we really want to know is what determines if an individual ends up on the AD path, which might have been decided earlier than we previously thought, given that the changes can be seen in some people as young as 45 years of age.…More
What this means for the biology of the AD brain is of interest. I think it makes sense that we observe typical aging signatures in AD brain, for example we expect accumulation of damage and decreased function in a normal brain over time. Certain processes will change, such as the activity of immune processes as they clear damaged cells or other aggregations from the brain in an attempt to boost neuron function, which slowly diminishes with age. When AD starts, these same processes are also active, trying to deal with the situation in the brain, in perhaps a similar way to what occurs, albeit more slowly, in the aging process.
In our studies of postmortem dementia brains, we see these natural aging processes in AD brains, but also in other forms of dementia or in brains undergoing some other form of neurodegeneration. We consider these processes "specific" for those diseases. They are a consequence of the brain state, whereas we typically want to know what specifically causes the start of these diseases, because that is what we want to prevent or halt. This study may help us identify these "normal" non-specific changes that occur in diseased or aging brains, and separate them from the other changes that occur in specific disease states, providing much clearer views of what happens there. This study is very helpful from that perspective.
Make a Comment
To make a comment you must login or register.