Could Tau PET Replace Amyloid Biomarkers as a Diagnostic for AD?
Quick Links
The particular type of tangle found in Alzheimer’s is unique to this disease, making tau PET a highly specific marker. In the May 11 JAMA Neurology, researchers led by Oskar Hansson at Skåne University Hospital in Malmö, Sweden, reinforce this point. In a large observational cohort, the second-generation tau tracer RO-948 outperformed both cerebrospinal fluid markers and MRI at telling AD dementia apart from other neurodegenerative disorders and from healthy aging. “You get higher specificity with tau PET than with amyloid markers,” Hansson told Alzforum. Because every person with a positive tau PET scan also had amyloid plaques, tau scans may eventually obviate the need to check amyloid status to diagnose AD, he suggested.
- Tau tracer RO-948 uptake is highly specific for Alzheimer’s dementia.
- Tau PET could supplant amyloid PET and CSF as an AD diagnostic.
- At the prodromal stage, however, CSF picks up more cases than tau PET.
However, this is not the case at earlier, prodromal stages. Because tangles form late in the disease course, CSF biomarkers performed better than tau PET at that stage.
"This is a milestone paper in establishing tau PET, and specifically RO-498 PET, as a clinically useful biomarker for patients attending Memory clinics," Bernard Hanseeuw of Massachusetts General Hospital wrote to Alzforum (full comment below).
Tobey Betthauser at the University of Wisconsin-Madison School of Medicine noted that this is one of the largest studies to date to examine differential diagnosis with tau PET. “This study presents a tremendous step forward for understanding the clinical and research utility of RO-948 and tau PET imaging,” he wrote to Alzforum (full comment below).

Only in Alzheimer’s. Tau tracer RO-948 lights up symptomatic AD brain (top right), and shows a smaller signal in prodromal AD (bottom middle). Even amyloid-positive but cognitively normal people show a hint of signal (bottom left), but amyloid-negative controls and other disorders do not. [Courtesy of Leuzy et al., JAMA Neurology.]
Most current tau tracers recognize the paired helical filaments of 3/4R tau found in AD brain, but not other types of tau aggregate (Feb 2020 conference news). In keeping with this, Hansson and colleagues had previously reported that flortaucipir distinguished AD from other disorders with about 90 percent sensitivity and specificity (Sep 2018 news). However, flortaucipir has off-target binding in the basal ganglia, choroid plexus, and temporal lobe, which sometimes muddies results. Next-generation tau tracers such as RO-948 are reputed to be cleaner.
The authors evaluated RO-948 scans from 613 participants in the Swedish BioFinder-2 observational cohort, whose average age was 69. First author Antoine Leuzy at Lund University, Sweden, analyzed cross-sectional data from 257 cognitively healthy controls, 154 people with mild cognitive impairment, 100 with AD dementia, and 102 with another neurodegenerative disorder. About 40 percent of controls and non-AD patients had amyloid plaques, as did about 60 percent of the MCI group, making amyloidosis a poor discriminator of these groups.
The tau tracer RO-948, on the other hand, was highly specific for AD dementia. Its uptake in Braak regions I-IV distinguished AD from non-AD disorders with an area under the curve of 0.97. The AUC measure estimates the accuracy of a diagnostic test by taking into account the test’s rate of both false negatives and false positives. Broken out, the tracer’s sensitivity and specificity were 92 and 91 percent, respectively, similar to the previous findings with flortaucipir. Tau PET was equally effective at picking out AD patients from healthy controls, with an AUC of 0.98 and sensitivity and specificity of 91 and 95 percent, respectively (see image above).
Compared with these tau PET findings, CSF Aβ42/40 topped out slightly lower, posting an AUC of 0.93 for distinguishing AD from other disorders, and 0.91 versus healthy controls. While CSF biomarkers were highly sensitive, they lacked specificity for AD, leading to many false positives.
MRI measures fared worse. Temporal lobe thickness achieved an AUC of 0.80 for discriminating AD from other disorders, while whole-brain cortical thickness reached 0.91 for separating AD dementia from healthy controls.
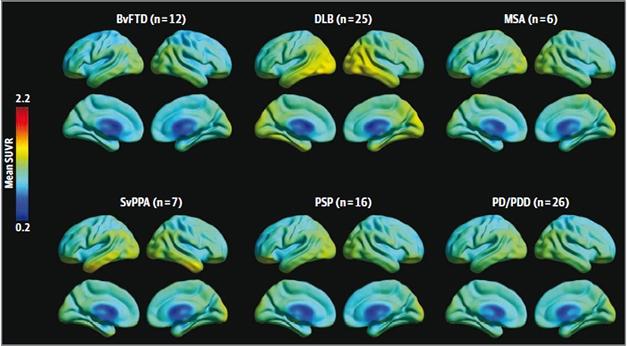
Tangles in DLB. RO-948 binds to some DLB brains (top middle), reflecting Alzheimer’s-type tangles there. The tracer has very low off-target binding to the temporal lobe in svPPA (bottom left). [Courtesy of Leuzy et al., JAMA Neurology.]
How about other neurodegenerative diseases? Twelve participants with behavioral variant frontotemporal dementia, 16 with progressive supranuclear palsy, 26 with Parkinson’s disease, six with multiple system atrophy, and 10 people with vascular dementia did not bind this tracer in their brains. On the other hand, 25 people with dementia with Lewy bodies did retain some tracer in their temporal and lateral parietal cortices (see image above). AD proteopathy is common in DLB, and indeed, 15 of the 25 had amyloid plaques, as well. Only those DLB participants with plaques took up the tracer, suggesting this was an on-target signal. Unsurprisingly, RO-948’s specificity for distinguishing DLB from AD was low, at 70 percent.
For another disorder, off-target binding was a problem. Seven people with semantic-variant primary progressive aphasia had some RO-948 uptake in the temporal pole. Because people with this disorder do not develop tau tangles, this was likely nonspecific binding. It is unclear what the tracer binds to, although binding was associated with white matter and could reflect astrocytosis, Hansson suggested. All svPPA participants fell below the cutoff for positivity with RO-948, which was set at 2.5 standard deviations above the average value in healthy young controls. Curiously, for temporal regions, this cutoff ended up at about 1.36 SUVR for RO-948 as well as for flortaucipir and MK-6240. “The cutoff seems to be surprisingly stable between different cohorts and tracers. That’s a very good thing for clinical implementation,” Hansson said.
Flortaucipir lights up svPPA brain as well, with uptake in the temporal lobe and cortex. In this study, the researchers directly compared RO-948 and flortaucipir in three participants who underwent scans with both tracers, and found RO-948 to be much cleaner. Even though the overall diagnostic accuracy with both tracers is similar, the lower off-target binding with RO-948 would be an advantage in specific cases such as svPPA patients, Hansson noted. Flortaucipir also binds off-target to choroid plexus, and this signal can spill over into the hippocampus, a key location for tangle pathology, he added. “There might be fewer false positives with RO-948,” Hansson speculated.
Notably, across the whole cohort, RO-948 retention indicated the presence of amyloid plaques with almost perfect accuracy. Only two people without plaques had high tau tracer uptake in Braak regions I and II. Both carried the MAPT R406W mutation, which gives rise to tangles. Two other amyloid-negative participants were barely over the threshold for tau positivity in Braak regions I and II. This could reflect primary age-related tauopathy, or noise in the data, the authors noted.
Because plaques and tangles were so highly concordant, and because tangles more closely track cognitive decline, tau PET scans could become the primary diagnostic tool for AD dementia, the authors proposed. If the tau PET scan is negative, clinicians could then use other tools such as FDG PET, dopamine imaging, and MRI to evaluate the likelihood of FTD, DLB, and vascular dementia, respectively.
So far, no tau tracers have been approved by the U.S. Food and Drug Administration, though a decision for flortaucipir is pending (May 2020 news). RO-948 is currently only available for research studies. Edilio Borroni at Roche told Alzforum that the company has not yet decided whether to develop RO-948 or the similar second-generation tracer, Genentech’s GTP1, for clinical use.
Although tau PET seems well-suited to detect AD dementia, the MCI stage of the disease is a different story. Here, it is not sharp enough. In the BioFinder-2 cohort, RO-948 identified MCI with an AUC of 0.80, sensitivity of 38 percent, and specificity of 95 percent. At this stage, CSF Aβ42/40 did well, posting an AUC of 0.89, with 100 percent sensitivity and 64 percent specificity. This fits with prior findings suggesting that CSF picks up Alzheimer’s pathology sooner than PET scans do (Aug 2016 conference news).
“More sensitive tau imaging agents, capable of capturing small increments of tau tangles, are still desirable,” noted Tharick Pascoal at McGill University, Montreal (full comment below).
Hansson suggested that longitudinal tau imaging might improve the ability of these scans to pick up early AD cases, since researchers could look for accumulation in early Braak regions, rather than using a brain-wide cutoff for tau positivity. In future work, Hansson and colleagues are investigating whether they can predict the best brain regions to monitor for future tangle accumulation based on a person’s baseline tau PET scan. This would also improve sensitivity.—Madolyn Bowman Rogers
References
News Citations
Further Reading
Primary Papers
- Leuzy A, Smith R, Ossenkoppele R, Santillo A, Borroni E, Klein G, Ohlsson T, Jögi J, Palmqvist S, Mattsson-Carlgren N, Strandberg O, Stomrud E, Hansson O. Diagnostic Performance of RO948 F 18 Tau Positron Emission Tomography in the Differentiation of Alzheimer Disease From Other Neurodegenerative Disorders. JAMA Neurol. 2020 Aug 1;77(8):955-965. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
University of Pittsburgh
This is an elegant, well-powered study evaluating the diagnostic performance of the novel tau tracer [18F]RO948. The analysis was very well-executed and gave the readers a fair overview of the tracer's binding characteristics in a clinical population. The authors reported, using their impressive BioFINDER dataset, that [18F]RO948 was able to differentiate AD dementia from cognitively unimpaired elderly and other neurodegenerative conditions with remarkable accuracy (AUC > 95 percent). This article also provided a comprehensive assessment of the tracer performance in relation to CSF and MRI markers. [18F]RO948 performed better than both CSF and MRI.
These results support that [18F]RO948 has the potential to differentiate AD dementia from other neurodegenerative conditions in research and clinical settings. The possible applications of [18F]RO948 as a surrogate endpoint for trials will be understood with the future availability of longitudinal data.
[18F]RO948 results are in line with previous reports using [18F]Flortaucipir, which also presented great performance (AUC >~0.92-0.95) to differentiate AD dementia from other neurodegenerative diseases (Ossenkoppele et al., 2018).
An apparent limitation was the reduced sensitivity of [18F]RO948 to detect tau accumulation confined to brain regions corresponding to early Braak stages compared to what was predicted by postmortem series (Braak and Braak, 1997). This limited sensitivity to the early detection of tau tangles was also reported for [18F]Flortaucipir (Schwarz et al., 2016; Lowe et al., 2019). Thus, more sensitive tau imaging agents, capable of capturing small increments of tau tangles, are still desirable. The possible contributions of the other second-generation tau tracers (e.g. [18F]MK-6240 and [18F]PI-2620) will be clarified by large studies across the disease continuum using these tracers.
References:
Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging. 1997 Jul-Aug;18(4):351-7. PubMed.
Lowe VJ, Lundt ES, Albertson SM, Min HK, Fang P, Przybelski SA, Senjem ML, Schwarz CG, Kantarci K, Boeve B, Jones DT, Reichard RR, Tranovich JF, Hanna Al-Shaikh FS, Knopman DS, Jack CR Jr, Dickson DW, Petersen RC, Murray ME. Tau-positron emission tomography correlates with neuropathology findings. Alzheimers Dement. 2020 Mar;16(3):561-571. Epub 2020 Jan 4 PubMed.
Ossenkoppele R, Rabinovici GD, Smith R, Cho H, Schöll M, Strandberg O, Palmqvist S, Mattsson N, Janelidze S, Santillo A, Ohlsson T, Jögi J, Tsai R, La Joie R, Kramer J, Boxer AL, Gorno-Tempini ML, Miller BL, Choi JY, Ryu YH, Lyoo CH, Hansson O. Discriminative Accuracy of [18F]flortaucipir Positron Emission Tomography for Alzheimer Disease vs Other Neurodegenerative Disorders. JAMA. 2018 Sep 18;320(11):1151-1162. PubMed.
Schwarz AJ, Yu P, Miller BB, Shcherbinin S, Dickson J, Navitsky M, Joshi AD, Devous MD Sr, Mintun MS. Regional profiles of the candidate tau PET ligand 18F-AV-1451 recapitulate key features of Braak histopathological stages. Brain. 2016 May;139(Pt 5):1539-50. Epub 2016 Mar 2 PubMed.
University of Wisconsin-Madison School of Medicine and Public Health
This study represents an impressive undertaking by the BioFINDER-2 team. It represents the largest RO-948 study published to date, and one of the largest studies investigating the ability of tau PET imaging to differentiate clinical phenotypes. Among the key findings, and perhaps unsurprisingly based on in vitro and first-in-human studies, RO-948 appears to be highly specific to tau aggregates observed in Alzheimer’s disease. This is best supported by the observation that across all clinical groups with rare exceptions (notably including R406w mutation carriers that are known to have mixed 3R and 4R paired-helical filamentous tau aggregates), elevated RO-948 binding was generally only observed in those that were positive for beta-amyloid. Thus RO-948 adds to a growing list of tau PET tracers like FTP, MK-6240, GTP-1, and others that seem to primarily target AD tau aggregates.
This study undoubtedly plays a role in advancing the field’s understanding of the clinical utility of tau PET imaging, and specifically RO-948 in the context of CSF AD biomarkers and other clinical phenotypes. Comparisons between RO-948 and CSF AD biomarkers suggest that RO-948 has the highest specificity for differentiating AD dementia from controls and non-AD disorders, but differentiating the pre-dementia stages of AD from controls and non-AD disorders might be better informed by markers of beta-amyloid. While these findings might suggest that RO-948 may not be as useful in staging preclinical and prodromal disease, more work in these populations is needed to ascertain this point more conclusively. In comparison to a recent FTP study, RO-948 seems to perform comparably to FTP for differentiating AD dementia from non-AD dementia and controls.
Of course when talking about tau tracers, it is nearly impossible to not discuss off-target binding and the potential for these ligands to have utility in non-AD tauopathies. Regarding the latter point, this study observed elevated anterior temporal FTP binding in three svPPA cases consistent with previous observations in the FTP literature. Of remarkable value to the field, these cases were also scanned with RO-948 allowing for direct comparison of FTP and RO-948 in a clinical phenotype most often associated with TDP-43 pathology. While they did observe some elevated RO-948 binding in these patients, the binding was generally lower than FTP and also differed spatially between the tracers.
Whether or not either of these tracers are binding to underlying TDP-43 pathology or other molecular target(s) will likely need to be resolved as imaging-to-postmortem cases become available and their underlying pathology is known. Regarding off-target signal, the authors did observed extra-axial RO-948 signal near the skull and meninges in a little over 4 percent of the sample. While FTP generally does not exhibit this signal, it has been observed previously in MK-6240 studies. In the present study, the extra-axial RO-948 signal did not impact clinical classification. Also of note is that neither RO-948 nor MK-6240 exhibit off-target binding in the basal ganglia.
This study presents a tremendous step forward for understanding the clinical and research utility of RO-948 and tau PET imaging, but there is still a clear need to develop PET ligands and/or fluid-based assays that are sensitive and selective to non-AD tauopathies and other protein aggregates observed in neurodegenerative disease. In addition to the currently available beta-amyloid and tau PET ligands, these precision tools will play a crucial role in the treatment of patients and the development of disease-modifying therapies.
Cliniques Universitaires Saint-Luc and Massachusetts General Hospital
This is an excellent paper from the BioFINDER-2 study team. Using their large sample size, they demonstrate the high specificity of RO-948 for confirming a diagnosis of AD in patients presenting with amnestic dementia. They found that a temporal ROI (Braak I-IV) performed slightly better than a neocortical ROI (Braak V-VI), and that tau-PET performed better than CSF or MRI to distinguish patients with AD dementia from either patients with non-AD neurodegenerative disorders or elderly controls. This is a milestone paper in establishing tau-PET, and specifically RO-498 PET, as a clinically useful biomarker for patients attending memory clinics.
Very interestingly, CSF biomarkers performed better than RO-948 PET to distinguish Aβ-positive MCI from either non-AD patients or controls, highlighting the (relative) lack of sensitivity of RO-948 for AD tauopathy in the prodromal stage of AD. Based on this data, if a single biomarker should be performed to confirm an AD diagnosis in a patient, clinicians should ask for tau-PET in demented patients but CSF in patients with MCI.
The key question that is not fully addressed in the paper is the reason for the superiority of CSF in MCI. Would amyloid measures (including amyloid PET) be better at that earlier stage given that tau is not consistently elevated yet ? Would fluid biomarkers be more suitable than PET measures given that fluid reflects a dynamic, ongoing, process while PET reflects the cumulative burden of past lesions (which may still be relatively low in some MCI cases) ? Longitudinal follow-up will be key here to determine which biomarker best predicts subsequent progression to dementia.
Improving the sensitivity of tau-PET to early tauopathy is a critical step for advancing the field. Further research should test lower thresholds in the early Braak stages ROIs, compare the sensitivity of RO-498 to other tau tracers, and evaluate how longitudinal PET data could help us detect earlier the individuals who will rapidly progress to dementia.
Growing evidence indicates that the different tau tracers have distinct sensitivities and off-target bindings. Head-to-head comparisons between these tracers, as the one provided here by the BioFINDER study in three svPPA patients, will definitely permit clinicians to select the most appropriate tau-PET tracer for each individual patient, according to clinical diagnosis and stage of disease. As acknowledged by the authors, final validation should be provided by a “ground truth,” which can either be clinical (dementia progression) or pathological (in PET-autopsy studies), both of which are still to be conducted for most tau PET tracers.
Make a Comment
To make a comment you must login or register.