Philadelphia: Diagnosis Light—Toward Infrared Plaques
Quick Links
If you’ve ever shone a flashlight through your hand and noticed what comes out on the other side, you have seen for yourself why red light could, in theory, make a medium for live diagnostics: It transmits better through thick, scattering human tissue than other parts of the visible spectrum. Brian Bacskai and colleagues at Massachusetts General Hospital in Charlestown, with collaborators at other institutions, have seized on this summer camp observation and are trying to develop an optical Alzheimer’s diagnostic. The researchers are not nearly there yet, but last week at the 9th International Conference on Alzheimer's and Related Diseases in Philadelphia, Bacskai briefed colleagues on how far they have gotten to date. “This would be a completely new approach,” Bacskai said.
Amyloid and tangle imaging agents including PIB (see ARF related Philadelphia story) and other compounds are under study at centers throughout the world. They hold great promise, but even if they progress through development and validation without major hiccups, they share the drawbacks of nuclear medicine. They require injection of radioactive compounds into a person’s blood and currently use positron emission tomography, or PET, which is expensive and not widely available. What if the same result could be achieved, more simply and cheaply, with optical techniques? One added advantage of optical imaging would be that an existing wealth of knowledge on the clever design of reagents might enable the synthesis of a highly sensitive probe, Bacskai added.
This project relies on near-infrared (NIR) laser scanning techniques to detect amyloid-binding reagents that fluoresce with wavelengths in the NIR spectrum. This differs from the multiphoton microscopy with which this research group has been imaging amyloid for a while (see ARF related news story). Multiphoton microscopy requires that the scientists make an opening in the mice’s skulls, and it can image tissue only in that small patch of brain up to about 500 microns deep. NIR imaging would be non-invasive and cover the whole brain, similar to PET or MRI. Indeed, NIR optical imaging is already being used in humans to detect breast cancer, visualize cerebral blood flow, and guide surgery.
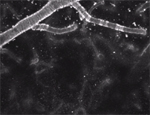
(Click on the image to see the movie)This is a 3-dimensional volume of brain (615x615x 200micron) in an anesthetized Tg2576 mouse, recorded over time with multiphoton microscopy. A bolus injection of a novel long-wavelength amyloid binding contrast agent was administered via tail vein. The compound appears in the cerebral circulation, crosses the blood-brain barrier, and labels the cerebral amyloid angiopathy in this mouse brain within minutes. The goal is to develop even longer-wavelength fluorescent ligands for Abeta to allow non-invasive optical detection of amyloid plaques in vivo using near- infrared spectroscopy. (Image credit to Jesse Skoch and Brian Bacskai)
How far along is this project? The work focuses mostly on two parts: designing reagents and devising the detection schemes. The detection hardware is mostly in place, Bacskai said. Using commercially available instruments and NIR fluorescent reagents coupled to Aβ antibodies, the researchers performed proof-of-principle experiments in brain slices and whole brain. These showed that the scientists can detect a fluorescent signal deep in the brain and that it correlates with the mouse’s brain Aβ burden.
The next step is to synthesize a real-life diagnostic agent. It must cross the blood-brain barrier, target amyloid deposits specifically, and emit NIR light. This is what consumes most of the effort now, said Bacskai. Of the candidate compounds Bacskai described, some get into the brain and have high affinity for amyloid deposits, but their fluorescent wavelength is not far enough in the infrared (see movie above). Others are specific and fluoresce properly, but do not cross the BBB. None fill all three criteria yet. Stay tuned.—Gabrielle Strobel.
Updated 8 September 2005:
Last month, the researchers reported initial results from their collaboration with chemist Timothy Swager, Massachusetts Institute of Technology. According to the paper, the scientists developed a marker that binds to plaques and then fluoresces when exposed to radiation in the near-infrared range.
References
News Citations
- Philadelphia: All Eyes on PIB Imaging—Is It Coming Along?
- Amyloid Ligand Looks Suited for Future Diagnostic Test
Other Citations
Further Reading
Primary Papers
- Nesterov EE, Skoch J, Hyman BT, Klunk WE, Bacskai BJ, Swager TM. In vivo optical imaging of amyloid aggregates in brain: design of fluorescent markers. Angew Chem Int Ed Engl. 2005 Aug 26;44(34):5452-6. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.