Amyloid Pompoms Decorate Capillaries in APP23 Mice
Quick Links
A new study shows striking images of early amyloid deposits on blood vessels of young APP23 transgenic mice, including pompom-like and cube-shaped clumps clinging to brain microvessels and distorting them. Older mice displayed holes in the vasculature around plaques with evidence of angiogenesis around the cleared areas. Published February 27 in PNAS online, the images come from Thomas Krucker and colleagues of the Novartis Institutes for Biomedical Research in Cambridge, Massachusetts. The scientists used vascular casting and scanning electron microscopy to reveal the three-dimensional architecture of microvessels in APP-expressing mice. Their work demonstrates that, in this mouse strain, damage to the microvasculature begins well before the onset of parenchymal amyloid plaques or vascular amyloid deposition. The authors suggest that imaging vascular alterations could be used as a biomarker of Alzheimer disease.
Changes in blood flow are a constant feature in AD, and are generally thought to be related to the widespread vascular pathology observed in AD brain. Krucker and colleagues have previously shown that older APP23 mice, which carry a human APP transgene with the Swedish mutation, have structural changes in blood vessels and modified blood flow (Beckmann et al., 2003; also see ARF related news story). In the current study, first authors Eric Meyer and Alexandra Ulmann-Schuler set out to define the progression of those changes over time, starting with young mice.
To visualize the vasculature of the whole brain, the investigators used corrosion casting, which involves infusing a polyurethane-based resin into the brain, letting it solidify and then removing the soft tissue. The result is a rubberized three-dimensional reproduction of the brain’s blood supply, right down to the capillary microvessels. In a modification of the technique, the researchers also used a novel fluorescent resin and left the soft tissue intact to look at the relation of plaques to the vasculature.
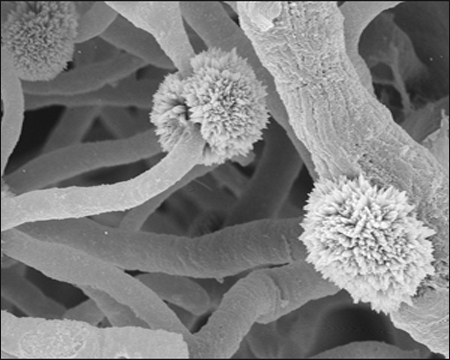
Pompoms of amyloid-β cling to blood vessel casts from 4-5-month-old APP transgenic mice. Image credit: Eric Meyer, Alexandra Ulmann-Schuler, and Thomas Krucker
In normal mice, casting revealed a regular network of vessels over the surface of the cortex. Casts from 18-month-old APP23 mice, on the other hand, showed a distinctly moth-eaten appearance, with holes dotting the cortex. Around the holes, which ranged from 0.03 to 3.5 mm in diameter, vessels were truncated, kinked, and studded with knob-shaped protrusions. At the hole edge, the vasculature was denser than usual, suggesting angiogenesis was occurring. By staining tissue with thioflavin S, the researchers showed that amyloid plaques sat in areas devoid of vasculature, suggesting that the holes seen in the casts corresponded to the location of plaques.
To trace the formation of the vascular gaps, the investigators made casts from mice from 4-5 months of age on. Even the youngest mice had significant numbers of holes, which increased with time up to 15 months of age. After that, the number of holes leveled off, but their size continued to grow.
Scanning electron microscopy of the casts revealed small knob-like structures attached to vessels in 3-month-old APP23 mice. The deposits, which turned out to be composed of Aβ peptides, took on a pompom-like appearance in 4-5-month-old animals (see image), with protruding spikes forming tufts 8 to 15 microns in size on small vessels. In some cases, the pompoms encircled capillaries and appeared to constrict or deform them. The researchers also saw smooth cubes of similar size on some vessels. The deposits stained with thioflavin, Congo red, and a polyclonal Aβ antibody. Mass spectroscopy identified Aβ peptides as the main component of the structures. No pompoms or cubes were seen in normal mice or any of several other strains of mice with mutations unrelated to AD. The present study reported only data in APP23 mice. However, Krucker told ARF by e-mail that the investigators had seen similar structures, though shifted toward older ages, in another APP transgenic mouse line, APP51 (Bodendorf et al., 2002. This paper covers primarily BACE transgenic mice. It mentions APP51 mice, the data on which have not been published elsewhere. The APP51 mice feature the same promoter as the APP23 mice, but express a wild-type human APP transgene.)
The authors speculate that pompoms may be starting points for amyloid deposition. Another recent imaging study that spied plaques forming in living mice (see ARF related news story) found that the deposits pop up near but not directly on blood vessels. That work did not visualize microvessels, however. Other studies have shown that in human brain, most small plaques are associated with capillaries (Kawai et al., 1990), and in several mouse models, plaques have been found exclusively in association with blood vessels (see ARF related news story). Vascular deposits that might be pompoms have also been described (Roher et al., 1993).
Based on their results, the authors propose a model where, they write, “minuscule amyloid deposits give rise to a local disturbance of the blood flow in capillaries, triggering a cascade of increased amyloid production/deposition resulting in vascular degeneration.” Ultimately, the process eats holes in the vascular net, accompanied by compensatory angiogenesis and remodeling. Local changes in blood flow could contribute to early behavioral changes that occur before plaque deposition, they speculate. The paper does not discuss what role Aβ oligomers versus plaques may play in this process. Even so, the early appearance of vascular disruptions supports the idea that impaired blood flow is a contributing cause of disease, and could provide a route to both early detection and monitoring of therapies, according to the authors.—Pat McCaffrey
References
News Citations
- Amyloid in Transgenic AβPP Mice Affects Blood Flow
- Popcorn Plaque? Alzheimer Disease Is Slow, Yet Plaque Growth Is Fast
- Amyloid-β—On or off the Wall?
Paper Citations
- Beckmann N, Schuler A, Mueggler T, Meyer EP, Wiederhold KH, Staufenbiel M, Krucker T. Age-dependent cerebrovascular abnormalities and blood flow disturbances in APP23 mice modeling Alzheimer's disease. J Neurosci. 2003 Sep 17;23(24):8453-9. PubMed.
- Bodendorf U, Danner S, Fischer F, Stefani M, Sturchler-Pierrat C, Wiederhold KH, Staufenbiel M, Paganetti P. Expression of human beta-secretase in the mouse brain increases the steady-state level of beta-amyloid. J Neurochem. 2002 Mar;80(5):799-806. PubMed.
- Kawai M, Kalaria RN, Harik SI, Perry G. The relationship of amyloid plaques to cerebral capillaries in Alzheimer's disease. Am J Pathol. 1990 Dec;137(6):1435-46. PubMed.
- Roher AE, Lowenson JD, Clarke S, Woods AS, Cotter RJ, Gowing E, Ball MJ. beta-Amyloid-(1-42) is a major component of cerebrovascular amyloid deposits: implications for the pathology of Alzheimer disease. Proc Natl Acad Sci U S A. 1993 Nov 15;90(22):10836-40. PubMed.
Other Citations
Further Reading
Papers
- Kumar-Singh S, Pirici D, McGowan E, Serneels S, Ceuterick C, Hardy J, Duff K, Dickson D, Van Broeckhoven C. Dense-core plaques in Tg2576 and PSAPP mouse models of Alzheimer's disease are centered on vessel walls. Am J Pathol. 2005 Aug;167(2):527-43. PubMed.
Primary Papers
- Meyer EP, Ulmann-Schuler A, Staufenbiel M, Krucker T. Altered morphology and 3D architecture of brain vasculature in a mouse model for Alzheimer's disease. Proc Natl Acad Sci U S A. 2008 Mar 4;105(9):3587-92. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
University of Texas at Austin
I have been a longtime admirer of Thomas Krucker’s vascular corrosion casting studies in mice, which resemble a 3-D micro-CT scan but are much more detailed and analyzable. They are especially useful when combined with magnetic resonance angiography imaging. In the present study, Krucker and his colleagues reveal changes observed in the cerebrovascular architecture of APP23 tg mice who were followed in an age-dependent time period lasting 25 months. During that time, parenchymal amyloid plaques appeared in the transgenic group, but only following significant microvascular changes. The slowly evolving microvascular pathology prior to plaque formation that the authors observed in the APP23 mice indicated to them that the disrupted microvessels ostensibly contribute to the early memory/learning deficits seen in this transgenic mouse model. The authors further conclude that early damage in the tg microvessels may worsen progressively over time, and could reflect the actual pathogenesis of AD, a point we have argued for many years (1).
These experimental observations confirm, and possibly explain, an increasing number of neuroimaging studies in humans that reveals preclinical reduced regional cerebral blood flow in people who later convert to AD (2). One caveat to be noted is that there is always a potential fallacy in assuming that gene mutation of APP or presenilins in mice or humans which produce excess Aβ also explain the pathological cascade seen in sporadic AD. This is a sophistic assertion that has gotten us into trouble for the last 20 years in our search for a cure to this dementia, and disregards the critical role of environmental risk factors to AD which are often present decades prior to plaque or tangle formation (3). However, having said that, there is evidence that brain hypoperfusion may trigger the expression of AD symptoms in people who carry the PS1 mutation (4), while hypoxia is reported to upregulate BACE1 (5).
References:
de la Torre JC, Mussivand T. Can disturbed brain microcirculation cause Alzheimer's disease?. Neurol Res. 1993 Jun;15(3):146-53. PubMed.
Caroli A, Testa C, Geroldi C, Nobili F, Barnden LR, Guerra UP, Bonetti M, Frisoni GB. Cerebral perfusion correlates of conversion to Alzheimer's disease in amnestic mild cognitive impairment. J Neurol. 2007 Dec;254(12):1698-707. PubMed.
Breteler MM. Vascular risk factors for Alzheimer's disease: an epidemiologic perspective. Neurobiol Aging. 2000 Mar-Apr;21(2):153-60. PubMed.
Johnson KA, Lopera F, Jones K, Becker A, Sperling R, Hilson J, Londono J, Siegert I, Arcos M, Moreno S, Madrigal L, Ossa J, Pineda N, Ardila A, Roselli M, Albert MS, Kosik KS, Rios A. Presenilin-1-associated abnormalities in regional cerebral perfusion. Neurology. 2001 Jun 12;56(11):1545-51. PubMed.
Sun X, He G, Qing H, Zhou W, Dobie F, Cai F, Staufenbiel M, Huang LE, Song W. Hypoxia facilitates Alzheimer's disease pathogenesis by up-regulating BACE1 gene expression. Proc Natl Acad Sci U S A. 2006 Dec 5;103(49):18727-32. PubMed.
View all comments by Jack de la TorreWeill College Medicine
The authors investigated the vascular alterations occurring in a mouse model of Alzheimer disease (AD) using corrosion casts and scanning electron microscopy. They report that APP23 mice exhibit structural alterations in cerebral microvessels before full-blown amyloid plaque deposition occurs. These alterations include formation of perivascular microdeposits, distortion, and remodeling of cerebral microvessels. As the accumulation of amyloid progresses, there are areas of loss of blood vessels that correspond to amyloid deposits and are surrounded by a halo of increased vascularization.
These observations provide a striking demonstration of the severe microvascular disruption in APP23 mice that develop well before the onset of cognitive decline. These highly restricted microvascular alterations fit well with the disruption in cerebrovascular regulation reported in APP mice. APP mice exhibit severe reduction in functional hyperemia, a vital homeostatic mechanism that matches local energy requirements with blood flow, and in the ability of cerebral microvessels to vasodilate in response to endothelial signals. The exquisite vascular localization of the early deposition fits well with these functional alterations.
However, recent studies demonstrate that the functional alterations in APP mice can be quickly counteracted by suppressing oxidative stress (Park et al., 2008) 2008). Therefore, the perivascular microdeposits described by Krucker et al. are unlikely to produce irreversible vascular damage. They may contribute to the dysfunction by, for example, being a source of vascular oxidative stress.
The recent Nature paper from the group of Brad Hyman (Meyer-Luehmann et al., 2008) did not identify the vessel wall as the first site of amyloid deposition, although a perivascular localization was found. The differences with the study of Krucker might be in the techniques used to detect amyloid deposits, i.e., corrosion casts vs. methoxy-XO4, and, most importantly, the transgenic animals used. Rapidly evolving imaging approaches in humans may provide data in AD and verify these provocative findings in animal models.
Overall, this is a nice study that provides a novel perspective of the microvascular disruption that occurs in a model of APP overexpression and Aβ accumulation.
References:
Park L, Zhou P, Pitstick R, Capone C, Anrather J, Norris EH, Younkin L, Younkin S, Carlson G, McEwen BS, Iadecola C. Nox2-derived radicals contribute to neurovascular and behavioral dysfunction in mice overexpressing the amyloid precursor protein. Proc Natl Acad Sci U S A. 2008 Jan 29;105(4):1347-52. PubMed.
Meyer-Luehmann M, Spires-Jones TL, Prada C, Garcia-Alloza M, de Calignon A, Rozkalne A, Koenigsknecht-Talboo J, Holtzman DM, Bacskai BJ, Hyman BT. Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer's disease. Nature. 2008 Feb 7;451(7179):720-4. PubMed.
View all comments by Costantino IadecolaMake a Comment
To make a comment you must login or register.