HAI—Aβ: First in Alzheimer’s Cascade, or Just Another Player?
Quick Links
Scientists worldwide now perform amyloid imaging on scores of research participants—from cognitively normal to demented—to figure out how Aβ buildup relates to other markers of neurodegeneration. Their findings are causing a small minority of scientists to question the amyloid cascade hypothesis anew. Does Aβ actually jumpstart a cascade that leads to neurodegeneration, or does it simply join a host of other toxic factors in wreaking havoc on the nervous system? At the 7th Human Amyloid Imaging Conference held 16-18 January in Miami, Florida, scientists presented some new data that support the latter view. They reported that other markers of neurodegeneration often precede evidence of Aβ plaques.
“AD-related neurodegeneration is probably a little more complicated than we thought it would be,” said Beth Mormino, a postdoctoral fellow from the lab of Reisa Sperling, Brigham and Women's Hospital, Boston, Massachusetts. “Not everything seems to be downstream of Aβ,” she said.
Mormino knew that as the brain ages, Aβ accumulates, the hippocampus shrinks, and episodic memory becomes worse. She wanted to know how those three things relate to each other in cognitively normal people. Does Aβ build up first? Mormino compared cross-sectional positron emission tomography (PET) scans using Pittsburgh compound B (PIB) with magnetic resonance imaging (MRI) analysis from 117 cognitively normal people, around age 73, from the Harvard Aging Brain Study. Smaller hippocampi tracked with advancing age better than did PIB status, suggesting age-related atrophy of the hippocampus can occur irrespective of amyloid accumulation. However, episodic memory had begun to fail only in those with evidence of brain amyloid. The results imply that amyloid weakens memory more than do other factors that contribute to hippocampal loss, Mormino suggested. Perhaps Aβ speeds the shrinking process or attacks a specific part of the hippocampus, she said. Alternatively, separate processes may attack the hippocampus all at once, and only when amyloid is also unleashed does memory suffer, she proposed. In any case, she proposed that Aβ is not the instigating factor in hippocampal volume loss. It is known that tau tangles accumulate in the hippocampus with age (Price and Morris, 1999), but Mormino was unable to assess the role of tau pathology in this mix of factors because tau tracers are not available just yet.
Miranka Wirth, from Bill Jagust’s lab at the University of California, Berkeley, found similar results in 72 cognitively normal people from the Berkeley Aging Cohort (BAC). Reduced hippocampal volume, impaired glucose metabolism, and thinner cortices all correlated with poorer cognitive function, regardless of PIB status. “We wouldn’t expect that based on the AD biomarker model proposed by Cliff Jack (see Jack et al., 2010, and Jack et al., 2013),” said Wirth. That model proposed a specific order of AD biomarker change, beginning with Aβ and ending with clinical decline. “We thought AD-related neurodegeneration would start with Aβ accumulation.” Aβ did seem to exert some influence, however. The relationship between the other biomarkers and cognition was stronger in those that bound more PIB. It implies that Aβ is not required to develop neurodegeneration, but aggravates existing neuronal trouble in cognitively normal older adults, Wirth told Alzforum.
Does Aβ mediate the relationship between cerebrovascular risk factors and gray matter demise in the same way? To find out, Sylvia Villeneuve, also from the Jagust lab, measured cortical thickness, hippocampal volume, and brain amyloid in 67 people from the University of Southern California Aging Brain Study. Volunteers were either cognitively healthy or had MCI, but all were at elevated risk for vascular disease. In both groups, lower HDL cholesterol (the good kind) and greater vascular burden (a higher number of risk factors, such as smoking, hypertension, diabetes, and cholesterol) correlated with thinner cortices. Low HDL cholesterol also associated with smaller hippocampi. In people with brain amyloid, those relationships were more robust, suggesting it worsened, but did not cause, the deterioration of gray matter. Thicker cortices seemed to bolster cognition against amyloid’s negative effects. “It suggests if you have a super thick cortex, amyloid will have less impact on cognition,” said Villeneuve.
While most of the talks focused on Aβ’s damage to gray matter, Kristen Kennedy, University of Texas at Dallas, looked at Aβ’s effect on white matter. Previous studies reported that human white matter connectivity degrades with age (see Kennedy and Raz, 2009), and that Aβ deposition further injures white matter tracts in mice (see Song et al., 2004). Kennedy thought amyloid might do the same in humans.
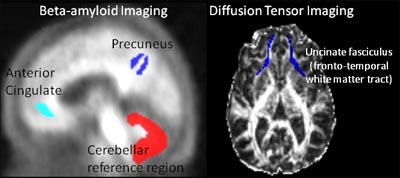
Diffusion tensor imaging (DTI) and florbetapir PET images supported that idea. In 141 healthy adults, aged 30-89, from the Dallas Lifespan Brain Study, more Aβ plaque in select regions correlated with poorer white matter integrity. For instance, amyloid in the anterior cingulate associated with damage to the nearby uncinate fasciculus (see image below). The researchers believe the DTI losses were mostly due to damaged myelin. “This study shows that Aβ is bad for connectivity,” Kennedy told Alzforum. “That suggests the peptide exerts some of its negative effects by limiting cross-talk and passage of information throughout the brain.”
Aβ and White Matter
Plaque in the anterior cingulate (light blue) leads to myelin breakdown nearby in the uncinate fasciculus. Image courtesy of Kristen Kennedy, University of Texas at Dallas
Taken together, the results present a picture that deviates slightly from the accepted amyloid cascade model. Aβ could be a partner in crime, rather than the singular mastermind behind neuron damage, said Wirth. “We all show that neurodegenerative patterns can be caused by many factors, including vascular risk, aging, and white matter damage,” she told Alzforum. “Those factors include Aβ, but it’s probably not the most prominent factor, at least in cognitively normal older subjects,” she added.
Experts batted these ideas around during discussion. “How much of our speculation about which comes first—neurodegeneration or amyloid, could be considered hot air because we’re measuring fibrillar, not soluble amyloid?” asked one commentator. That is an open question, said Victor Villemagne, University of Melbourne, Australia. “We know people have Aβ oligomers before plaque,” he said. (New Aβ oligomer ELISAs are detecting high amounts in brain tissue; see ARF related news story). Even if in-vivo imaging of those smaller aggregates is not yet possible, “we know that misprocessing of APP leads directly to Alzheimer’s disease,” so there must be some causative role for Aβ, Villemagne added.
Cliff Jack, Mayo Clinic, Rochester, Minnesota, partly agreed. “Genetic evidence is incontrovertible that an independent "Aβ-opathy" can induce or accelerate tauopathy—the reverse isn’t true,” he said. At the same time, he continued, “People are coming to this common conceptual idea of neurodegeneration independent of Aβ, including those of us at the Mayo Clinic,” he said (see ARF related news story). This kind of neurodegeneration could be tau mediated, unrelated to tau (from such factors as vascular disease), or both, he told Alzforum.
“I think this points out that we don’t really understand what aging is—it’s not as simple as just Aβ and tau,” Jagust said. Neurodegeneration happens in people without amyloid, so there must be something fundamental to systems that make them vulnerable to a whole panoply of factors, he said. “Amyloid is one, but not the only piece of the puzzle.”
Others wondered why the debate even mattered. “I think we should stop arguing about whether it’s Aβ or independent neurodegeneration—it’s both,” said Sperling. “We should find ways to work on the different processes therapeutically—we’ll probably need both Aβ and non-Aβ approaches to fix this disease.” Villemagne concurred, suggesting to Alzforum that neurodegeneration can probably arise three ways—due to Aβ alone, as a result of the peptide plus other factors, and independent of Aβ accumulation.—Gwyneth Dickey Zakaib.
References
News Citations
- New Assays for Aβ Oligomers—Spinal Fluid a Miss, Brain Awash
- HAI—Sharper Curves: Revamping a Biomarker Staging Model
Paper Citations
- Price JL, Morris JC. Tangles and plaques in nondemented aging and "preclinical" Alzheimer's disease. Ann Neurol. 1999 Mar;45(3):358-68. PubMed.
- Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, Petersen RC, Trojanowski JQ. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurol. 2010 Jan;9(1):119-28. PubMed.
- Jack CR, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, Shaw LM, Vemuri P, Wiste HJ, Weigand SD, Lesnick TG, Pankratz VS, Donohue MC, Trojanowski JQ. Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013 Feb;12(2):207-16. PubMed.
- Kennedy KM, Raz N. Aging white matter and cognition: differential effects of regional variations in diffusion properties on memory, executive functions, and speed. Neuropsychologia. 2009 Feb;47(3):916-27. PubMed.
- Song SK, Kim JH, Lin SJ, Brendza RP, Holtzman DM. Diffusion tensor imaging detects age-dependent white matter changes in a transgenic mouse model with amyloid deposition. Neurobiol Dis. 2004 Apr;15(3):640-7. PubMed.
Other Citations
Further Reading
Papers
- Förster S, Grimmer T, Miederer I, Henriksen G, Yousefi BH, Graner P, Wester HJ, Förstl H, Kurz A, Dickerson BC, Bartenstein P, Drzezga A. Regional expansion of hypometabolism in Alzheimer's disease follows amyloid deposition with temporal delay. Biol Psychiatry. 2012 May 1;71(9):792-7. PubMed.
- Kennedy KM, Raz N. Aging white matter and cognition: differential effects of regional variations in diffusion properties on memory, executive functions, and speed. Neuropsychologia. 2009 Feb;47(3):916-27. PubMed.
- Song SK, Kim JH, Lin SJ, Brendza RP, Holtzman DM. Diffusion tensor imaging detects age-dependent white matter changes in a transgenic mouse model with amyloid deposition. Neurobiol Dis. 2004 Apr;15(3):640-7. PubMed.
- Jack CR, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, Shaw LM, Vemuri P, Wiste HJ, Weigand SD, Lesnick TG, Pankratz VS, Donohue MC, Trojanowski JQ. Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013 Feb;12(2):207-16. PubMed.
News
- Dimmed Network Connections May Explain Metabolic Shortfall
- Multimodal Imaging: Structure, Function, Amyloid Not in Synch
- Miami: Diagnosis and Amyloid Scan Can Be at Odds
- Does ApoE4 Lower Brain Metabolism Independently of Aβ?
- API Echoes DIAN: Biomarker Changes Precede Symptoms by 20 Years
- New Assays for Aβ Oligomers—Spinal Fluid a Miss, Brain Awash
- HAI—Sharper Curves: Revamping a Biomarker Staging Model
- HAI—Standardizing Amyloid PET: The Centiloid Project
- HAI—Spotlight on Tau Tracers at Human Amyloid Imaging Meeting
- HAI—Amyloid Imaging in the Clinic: New Guidelines and Data
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.